CIT 2015:吡格列酮对支架内再狭窄的影响
2015-03-20 Tylen Chen 丁香园
第十三届中国介入心脏病学大会将在 2015 年 3 月 19-20 日召开,来自北京安贞医院的张明多博士等将在大会介绍关于一项 meta 分析研究——吡格列酮对冠脉药物洗脱支架植入术后支架内再狭窄的影响。 支架内再狭窄(ISR)目前仍是一种威胁生命的并发症,有研究表明吡格列酮可降低药物洗脱支架(DES)植入术后 ISR 的发病率。所以,张明多等开展了一项随机对照的 meta 分析研究,旨在评
第十三届中国介入心脏病学大会将在 2015 年 3 月 19-20 日召开,来自北京安贞医院的张明多博士等将在大会介绍关于一项 meta 分析研究——吡格列酮对冠脉药物洗脱支架植入术后支架内再狭窄的影响。
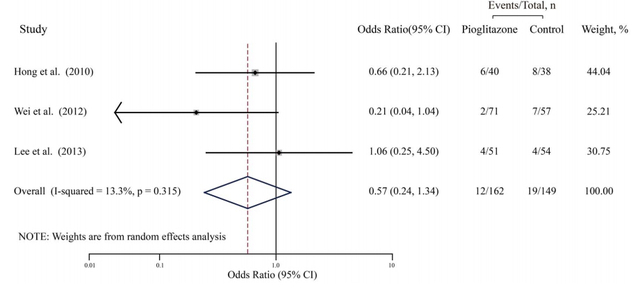
支架内再狭窄(ISR)目前仍是一种威胁生命的并发症,有研究表明吡格列酮可降低药物洗脱支架(DES)植入术后 ISR 的发病率。所以,张明多等开展了一项随机对照的 meta 分析研究,旨在评估吡格列酮治疗对冠脉药物洗脱支架植入术后支架内再狭窄的影响。

该研究为随机对照试验(RCT),系统性地回顾了 2014 年 5 月之前多个在线数据库的研究文章,还进一步搜索相关引文。主要终点是 ISR 的发生率,次级终点包括最小管腔直径、安置支架血管的狭窄分数、晚期支架脱落、支架内新生血管内膜体积、靶血管新生血管形成(TVR)、靶病变新生血管形成、心肌梗死、支架血栓形成和死亡。
结果显示:该 meta 分析研究纳入了 5 个研究,包括 255 例使用吡格列酮治疗患者和 245 例非吡格列酮治疗患者(作为对照组)。吡格列酮并没有显著降低 ISR 发生率,且异质性较低。次级结局方面,除了晚期支架脱落和 TVR,吡格列酮并没有持续影响这些终点事件的综合评估。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CIT#
36
#支架内再狭窄#
39
需要大样本
113
#吡格列酮#
34
#再狭窄#
40
整体样本量太小,研究也少,说服力不强
99