JAMA Neurol:药物洗脱支架能明显降低高级别ICAS患者支架内狭窄和卒中复发风险!(NOVA研究)
2022-01-05 MedSci原创 MedSci原创
与BMS相比,DES可降低有症状的高等级ICAS患者的ISR和缺血性卒中复发的风险。
支架内再狭窄(ISR)是使用标准裸金属支架(BMS)治疗的患者在颅内支架术后复发中风的主要原因。目前,有关药物洗脱支架(DES)是否能降低颅内动脉粥样硬化性狭窄(ICAS)的ISR风险仍不清楚。
为了研究DES是否能降低有症状的高等级ICAS患者的ISR和卒中复发的风险,来自我国首都医科大学天坛医院神经内科的专家开展了相关研究,结果发表在JAMA Neurology杂志上。
2015年4月27日至2018年11月16日,在中国16个颅内支架手术量大的医疗中心进行了一项前瞻性、多中心、开放标签的随机临床试验,并对结果进行盲法评估。有症状的高级别ICAS患者被随机纳入并随访1年。
患者被随机分配接受DES(NOVA颅内西罗莫司洗脱支架系统)或BMS(Apollo颅内支架系统)治疗,比例为1:1。主要疗效终点是手术后1年内的ISR,定义为植入支架内或紧邻支架(5mm内)的管腔直径大于50%的狭窄。主要安全终点是手术后30天内的任何中风或死亡。
结果共有263名参与者(194名男性[73.8%];中位[IQR]年龄,58[52-65]岁)被纳入分析,其中132人被随机分配到DES组,131人被分配到BMS组。总的来说,DES组的1年ISR率低于BMS组,总体风险降低76%(10 [9.5%] vs 32 [30.2%];OR=0.24;95% CI,0.11-0.52;P < .001)。
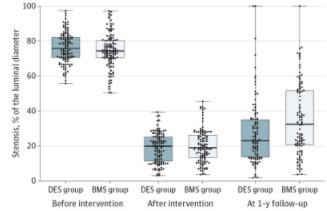
DES组和BMS组随访1年内支架内在狭窄风险差异
其中,DES组从第31天到1年的缺血性中风复发率也明显较低,风险降低90%(1 [0.8%] vs 9 [6.9%];HR=0.10;95%CI,0.01-0.80;P = .03)。但在DES组和BMS组之间,30天内任何中风或死亡的比率没有明显差异(10[7.6%] vs 7[5.3%];OR=1.45;95%CI,0.54-3.94;P=.46)。
综上,本试验发现,与BMS相比,DES可降低有症状的高等级ICAS患者的ISR和缺血性卒中复发的风险。
参考文献:
Jia B, Zhang X, Ma N, et al. Comparison of Drug-Eluting Stent With Bare-Metal Stent in Patients With Symptomatic High-grade Intracranial Atherosclerotic Stenosis: A Randomized Clinical Trial. JAMA Neurol. Published online January 04, 2022. doi:10.1001/jamaneurol.2021.4804
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#复发风险#
34
#Neurol#
25
#洗脱支架#
39
#药物洗脱支架#
51
#卒中复发#
30
#ICAS#
24
#Cas#
0
学习了
41
心血管新福利
43
已学
41