Front Cardiovasc Med:肺动脉高压的新型预后预测因子:血尿素氮
2021-11-12 刘少飞 MedSci原创
特发性肺动脉高压(IPAH)是一种危及生命的疾病,死亡率增加。尿素循环途径在IPAH的严重程度和治疗反应中起主要作用。血尿素氮 (BUN) 可作为IPAH预后的预测因子。

肺动脉高压 (PAH) 是一种罕见的进行性疾病,影响前毛细血管肺血管系统,其确切的潜在危险因素仍然未知。静息时肺动脉压力持续超过 25 mmHg,运动时持续超过 30 mmHg,这可能最终导致右心室 (RV) 衰竭和死亡。PH在世界卫生组织(WHO)分类系统中分为5个临床亚组,特发性肺动脉高压(IPAH)属于第1大类。
减少的一氧化氮 (NO) 被认为是 PAH 的重要发病机制。尿素循环提供精氨酸,然后精氨酸被一氧化氮合酶 (NOS) 转化为瓜氨酸、NO 和水 。在PAH患者,精氨酸酶的活性增加,然后用竞争NOS,导致精氨酸减少和NO的产生。精氨酸酶是一种可以将精氨酸转化为鸟氨酸和尿素的酶,它可以与 NOS 竞争精氨酸,导致 NO 表达降低。在实验性肺动脉高压大鼠中观察到尿素增加; 因此,有人提出尿素水平的增加可能与 PH 的进展有关。然而,关于与 PAH 进展和预后相关的尿素量知之甚少。
在本研究中,我们旨在调查血尿素氮 (BUN) 与PAH患者住院时间和重症监护病房 (ICU) 时间、住院死亡率、90 天死亡率和 4 年死亡率之间的关系。
研究方法:本研究采用回顾性队列研究设计。
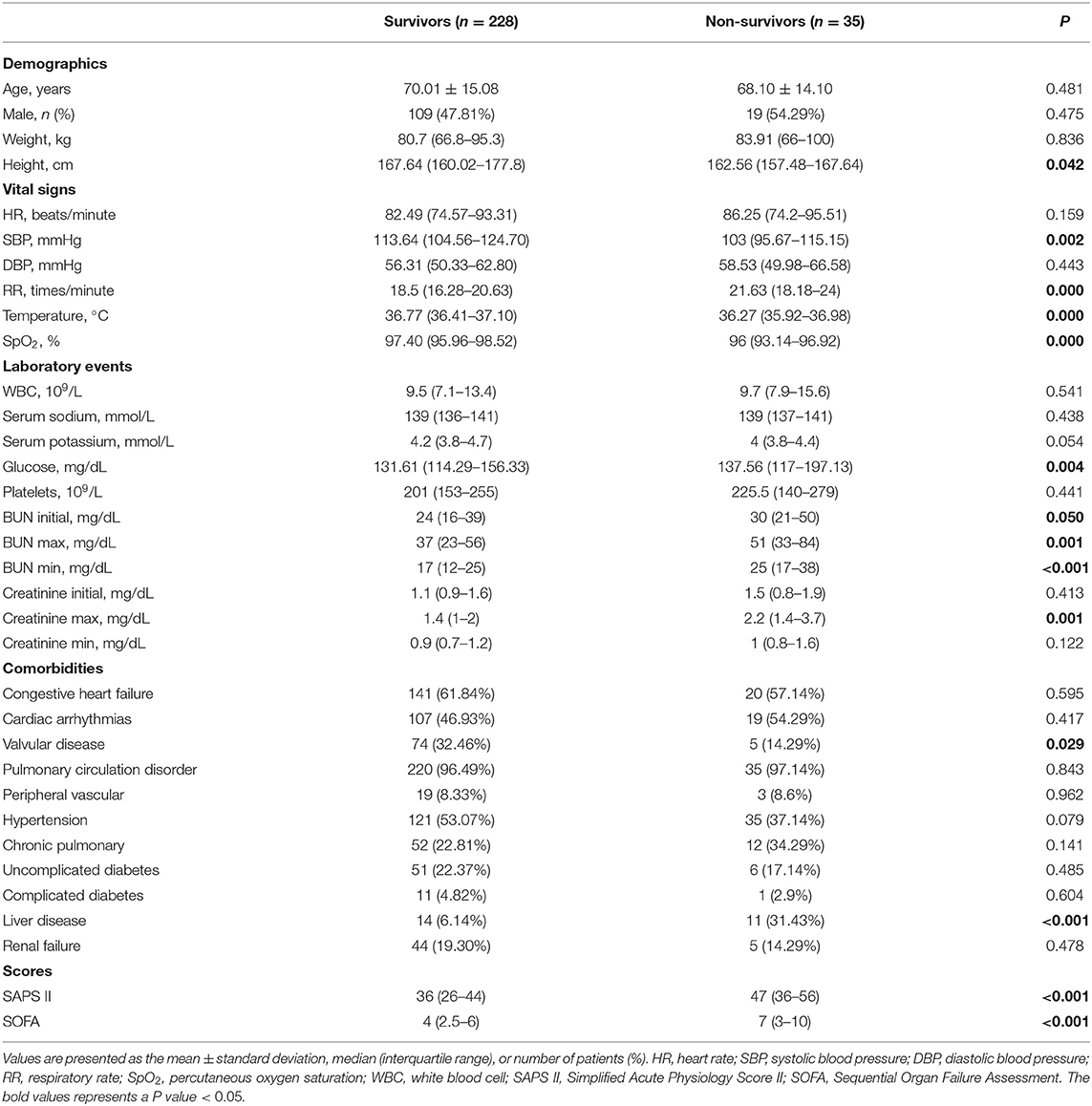
总共有 263 名符合选择标准的患者参加了我们的研究,其中 35 名患者(13.3%)在医院死亡。总结了入选患者的基线特征,包括人口统计学、生命体征、实验室事件、合并症和评分。
研究结果:
针对263名符合选择标准的患者进行数据分析。发现BUN与住院时间和 ICU 停留时间显着正相关(住院时间:ρ = 0.282,ICU 停留时间:ρ = 0.276;所有P < 0.001)。

在IPAH患者的较高 BUN 四分位数中观察到较高的医院、90 天和 4 年死亡率(医院:P = 0.002;90 天:P = 0.025;4 年:P < 0.001)。
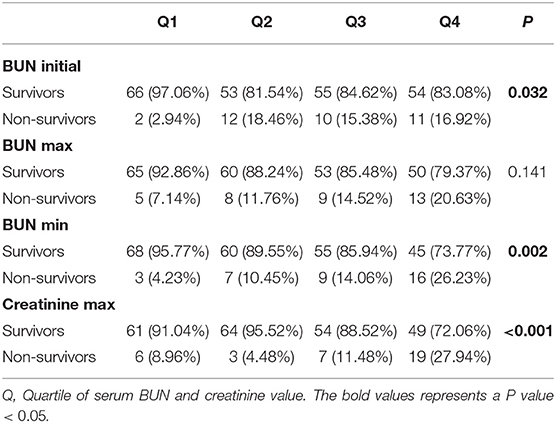
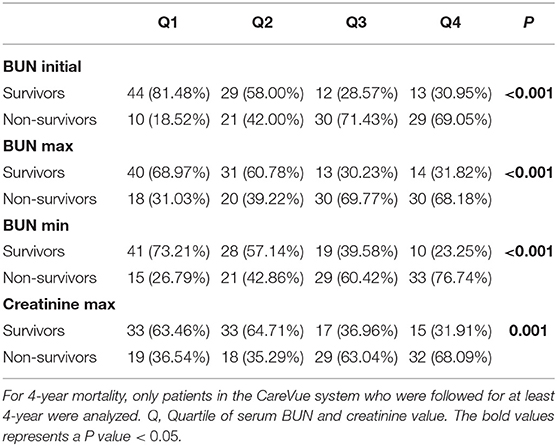
Kaplan-Meier 生存曲线显示,BUN 四分位数较高的患者 4 年生存率往往较低(Q1:7.65%,Q2:10.71%;Q3:14.80%,Q4:16.84%;P < 0.0001)。Logistic 回归分析发现 BUN 与死亡率显着相关(医院:OR = 1.05,95% CI = 1.02-1.08,P= 0.001; 90 天:OR = 1.02,95% CI = 1.00-1.05,P = 0.027;4 年:OR = 1.05,95% CI = 1.02-1.08,P = 0.001)。ROC和AUC结果显示BUN对死亡率的诊断性能中等。

研究结论:
BUN与PPH患者住院时间和ICU停留时间呈正相关。较高的 BUN 与较高的住院、90 天和 4 年死亡率以及IPAH患者较低的 4 年生存率相关。这些发现表明 BUN 可以成为IPAH的一种新的潜在预后预测因子。
文章出处:
Hu B, Xu G, Jin X, Chen D, Qian X, Li W, Xu L, Zhu J, Tang J, Jin X, Hou J. Novel Prognostic Predictor for Primary Pulmonary Hypertension: Focus on Blood Urea Nitrogen. Front Cardiovasc Med. 2021 Oct 25;8:724179. doi: 10.3389/fcvm.2021.724179. PMID: 34760940; PMCID: PMC8572959.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#尿素氮#
46
#ASC#
40
#动脉高压#
0
#预测因子#
49
#血尿#
44
#Med#
42