各种心功能分级,你都了解吗?
2016-06-11 吴鹏宇 医学界心血管频道
1、心功能分级与分度 按心衰发展的程度,即病人胜任体力活动的能力,结合临床表现一般将心功能分为四级,心衰分为三度: 2、凯氏(Killip)分级 它主要根据症状和体征,较简便易行。适用于急性心肌梗死并发心力衰竭的严重程度。 I级:指急性心肌梗死无心力衰竭,无肺部啰音,无舒张期奔马律,肺毛细血管楔嵌压可轻度升高; II级:有轻度至中度的心力衰竭,肺部有罗音,但不超过 50%,体检颈静脉怒张,可闻
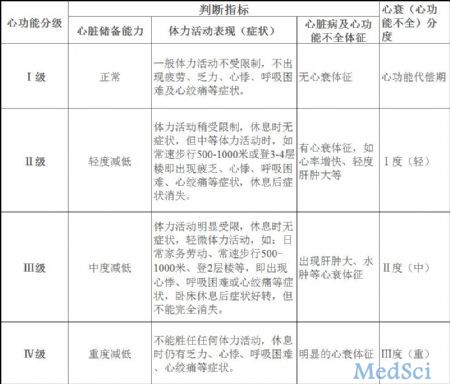
1、心功能分级与分度
按心衰发展的程度,即病人胜任体力活动的能力,结合临床表现一般将心功能分为四级,心衰分为三度: 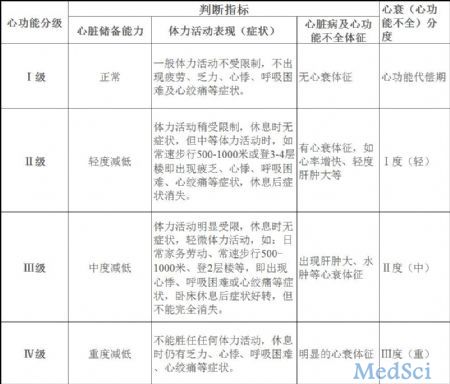
2、凯氏(Killip)分级
它主要根据症状和体征,较简便易行。适用于急性心肌梗死并发心力衰竭的严重程度。
I级:指急性心肌梗死无心力衰竭,无肺部啰音,无舒张期奔马律,肺毛细血管楔嵌压可轻度升高;
II级:有轻度至中度的心力衰竭,肺部有罗音,但不超过 50%,体检颈静脉怒张,可闻及舒张早期奔马律,胸部上有肺淤血表现;
III级:可出现急性肺水肿;Ⅳ级出现休克。
记忆口诀:一度一般没问题,二度啰音占一半,舒早奔马肺淤血,三度全罗肺淤血,四度休克来报道。
3、美国纽约心脏病学会(NYHA)1928年心功能分级(我国采用):
Ⅰ级: 患者患有心脏病但活动量不受限制,平时一般活动不引起疲乏、心悸、呼吸困难或心绞痛。
Ⅱ级:心脏病患者的体力活动受到轻度的限制,休息时无自觉症状,但平时一般活动下可出现疲乏、心悸、呼吸困难或心绞痛。
Ⅲ级:心脏病患者体力活动明显限制,小于平时一般活动即引起上述的症状。
Ⅳ级:心脏病患者不能从事任何体力活动。休息状态下也出现心衰的症状,体力活动后加重。
记忆口诀:纽约老大心眼坏,一年还能够生活,二年干活心虚喘,休息以后会好转;三年动动都难受,四年只能家里躺。
心衰是心脏病的最后的发展阶段。几乎所有的心脏病都可以引起心衰。根据心脏的受损部位可分为左心衰、右心衰和全心衰;根据发病的速度可分为急性心力衰竭和慢性心力衰竭;根据心力衰竭时心输出量的高低可分为收缩功能不全和舒张功能不全两种类型。
心衰的治疗
其药物选择要遵循低剂量、副作用小、联合用药、病人耐受性好易于接受的治疗常用药物主要有利尿剂、血管扩张剂、强心苷、血管紧张素转化酶抑制剂和血管紧张素Ⅱ受体拮抗剂、β1受体阻断剂等,其中强心苷为增强心肌收缩力的药物;利尿剂及血管扩张剂是降低心脏负荷的药物;血管紧张素转化酶抑制剂、血管紧张素Ⅱ受体拮抗剂与醛固酮拮抗剂可以作用于肾素-血管紧张素-醛固酮轴系统,减少血管紧张素Ⅱ生成和拮抗其缩血管作用,减少高醛固酮所引起的水钠潴留。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心功能#
36
归纳很好
98
已经收藏
62
学习学习!
131
基础
133
获取积分
95