AGING CELL:改变神经代谢可促进蛋白质稳态和长寿
2019-03-01 海北 MedSci原创
衰老与组织和代谢稳态的进行性丧失有关。已有的研究显示,这种损失可以通过单基因扰动延迟,从而延长寿命。但是至今为止,我们对于这种扰动如何影响代谢和保护机体网络,以延长寿命仍不清楚。
衰老与组织和代谢稳态的进行性丧失有关。已有的研究显示,这种损失可以通过单基因扰动延迟,从而延长寿命。但是至今为止,我们对于这种扰动如何影响代谢和保护机体网络,以延长寿命仍不清楚。
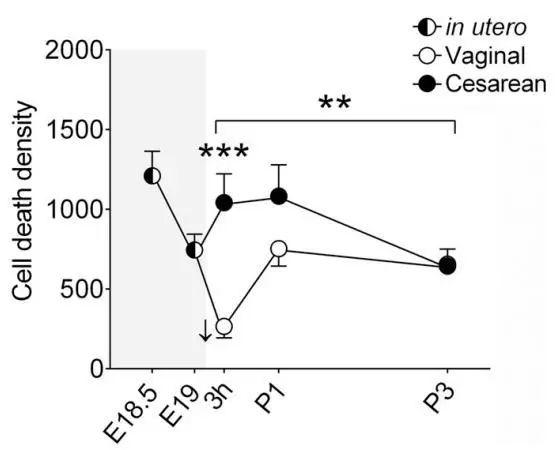
最近,研究人员通过全面描述果蝇大脑中蛋白质周转率的年龄相关变化,以及具有升高的Jun-N末端激酶信号传导的长寿动物的神经元代谢组,转录组和碳通量的变化来解决这个问题 。
研究人员发现,这些动物表现出延迟的年龄相关的蛋白质周转率的下降,以及稳态神经元葡萄糖-6-磷酸水平的降低,和由于葡萄糖-6-磷酸脱氢酶(G6PD)的诱导导致的进入戊糖磷酸途径的碳通量的增加。
在神经元中过度表达G6PD足以重现这些代谢和蛋白质稳态变化,并延长寿命。
因此,该研究确定了代谢变化与神经元中改善的蛋白质稳态之间的联系,这有助于长寿突变体的寿命延长。
原始出处:
Lifen Wang et al. JNK modifies neuronal metabolism to promote proteostasis and longevity. Aging Cell, 2019; doi: https://doi.org/10.1111/acel.12849
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
24
#白质#
38
#稳态#
40
#CEL#
33
#蛋白质#
28