J Evol Biol:研究发现精子质量与相貌负相关
2014-09-15 tencent 腾讯科技
看上去很英俊的男人,他的精子质量如何呢?这个问题听起来或许有点荒唐,但是一项最新研究已经证实,男性面貌吸引力和他们的精子质量之间存在联系:英俊阳刚样貌的男性拥有的精子质量不如其他男性。 研究的合著者,澳洲大学进化生物学研究中心的助理讲师Jukka Kekalainen博士在写给《赫芬顿邮报》的一封邮件中称:“据我们所知,这是第一次证实这一现象。”据纽约日报报道,尽管之前的研究已经表明高睾丸素水平
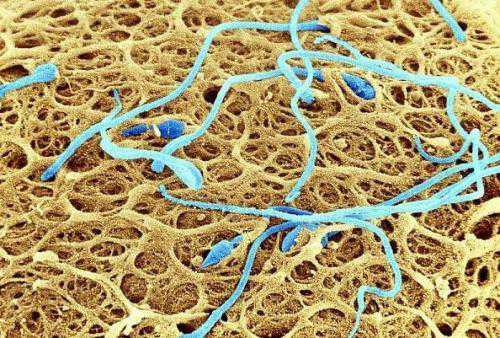
看上去很英俊的男人,他的精子质量如何呢?这个问题听起来或许有点荒唐,但是一项最新研究已经证实,男性面貌吸引力和他们的精子质量之间存在联系:英俊阳刚样貌的男性拥有的精子质量不如其他男性。
研究的合著者,澳洲大学进化生物学研究中心的助理讲师Jukka Kekalainen博士在写给《赫芬顿邮报》的一封邮件中称:“据我们所知,这是第一次证实这一现象。”据纽约日报报道,尽管之前的研究已经表明高睾丸素水平能够损伤精子的生成,但研究人员们并没有准备好解释他们的发现。
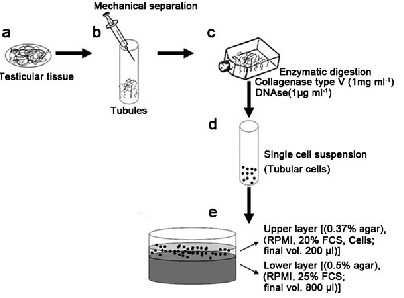
来自西班牙、澳大利亚和哥伦比亚的研究人员组成的团队进行了这项研究,他们对巴伦西亚大学的50位白种人学生志愿者进行了精液分析。接下来,这些男性的照片被展示给异性恋的男性和女性。女性调查者被要求从这些男性中选择出她们中意的长期配偶。男性调查者则被要求从中选择他们认为会被女性选中的照片。
研究人员同样对全部50位男性的面部特征进行了人体测量分析,测量了他们的眼睛大小、颧骨和鼻孔的宽度,以及之前研究鉴定为阳刚特征的其它部位。最后研究人员将这些男性的面部特征与男性精细胞的运动性、形态学和浓度进行了对比。
研究人员除了寻找阳刚面貌与精子质量之间的联系之外,还想要了解男性精子质量是否与他们的英俊存在联系。Kekalainen在邮件中写道:“我们发现它们之间确实存在联系。”
但是这是否意味着那些想要寻找能养育后代配偶的女性应当提防英俊的男性?或许并不需要如此,我们至少还需要寻找更多的证据。正如Kekalainen在邮件中说的:“在给予女性选择配偶的小窍门之前,我们还需要进行更多的研究来证实这一发现背后的原因和原理。”
原始出处
Soler C1, Kekäläinen J, Núñez M, Sancho M, Alvarez JG, Núñez J, Yaber I, Gutiérrez R.Male facial attractiveness and masculinity may provide sex- and culture-independent cues to semen quality.J Evol Biol. 2014 Sep
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Bio#
18
#研究发现#
25
#Biol#
18
#负相关#
19