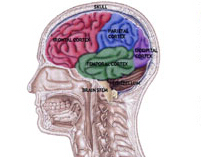
JAMA Surgery:脑损伤的治疗指南并不能保证更好的结果
2015-07-30 崔倩 译 MedSci原创
二十年前,脑外伤基金会(Brain Trauma Foundation)公布了其第一套治疗创伤性脑损伤的指南。 如今,洛杉矶创伤协会--其中包括一些来自于加州大学洛杉矶分校的医生--已经发现按照这些准则行事并不一定能为患者提供更好的结果。 该研究报告通过同行评审在线发表在JAMA Surgery杂志上,该协会分析了所有的14个
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GER#
23
#治疗指南#
20
#surgery#
29
好文
102
好文
76
好文
99
#损伤#
23