Heart:主动脉重度狭窄患者冠状动脉绝对流量及微血管阻力储备
2022-08-21 MedSci原创 MedSci原创
在重度主动脉狭窄和非阻塞性冠状动脉疾病患者中,随着左室肥厚的进展,静息血流增加的代偿机制维持了静息时的充分灌注,而在充血时则不存在。
主动脉狭窄导致的左心室肥厚发生发展伴随着适应性冠状动脉血流调节。近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员的目的是评估有无主动脉狭窄患者的绝对冠状动脉流量、微血管阻力、冠状动脉逆流(CFR)和微血管阻力储备。
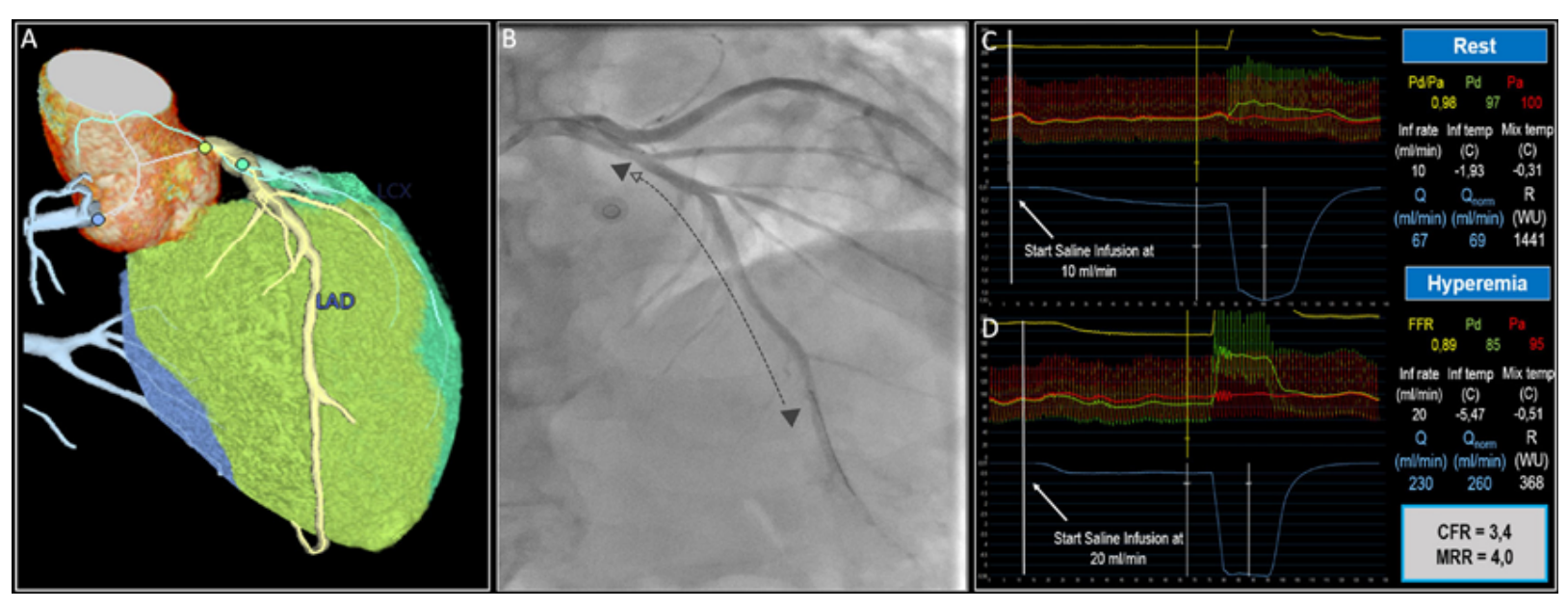
研究人员采用连续热稀释法测定了29例主动脉狭窄患者和29例非主动脉狭窄对照组的冠状动脉绝对流量和微血管阻力,并这些患者的年龄、性别、糖尿病和心外膜冠状动脉病变的功能严重程度进行了匹配。研究人员通过超声心动图和心脏CT检查定量测定了心肌做功、心肌总质量及左前降支特异性质量。
与对照组相比,主动脉狭窄患者左室重构明显阳性,整体纵向应变较低,整体工作效率较低。主动脉狭窄患者左室心肌总质量和LAD特异性心肌质量显著升高(p=0.001)。
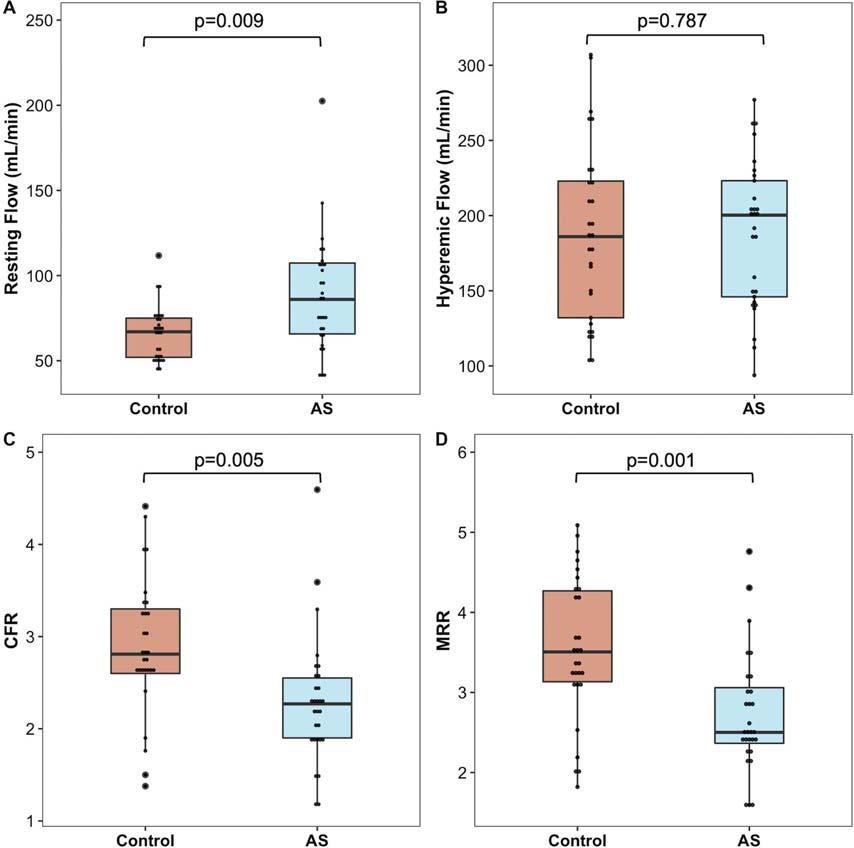
与对照组相比,主动脉狭窄组LAD的绝对静息血流显著增加(p=0.009),导致主动脉狭窄组的CFR和微血管阻力储备低于对照组(p均<0.005)。在充血流量、静息和充血阻力方面没有发现差异。主动脉狭窄组心肌充血灌注(以冠状动脉绝对流量与LAD之比来计算获得,以mL/min/g表示)显著低于对照组(p=0.035)。
由此可见,在重度主动脉狭窄和非阻塞性冠状动脉疾病患者中,随着左室肥厚的进展,静息血流增加的代偿机制维持了静息时的充分灌注,而在充血时则不存在。因此,CFR和微血管阻力储备都显著受损。
原始出处:
Pasquale Paolisso.et al.Absolute coronary flow and microvascular resistance reserve in patients with severe aortic stenosis.heart.2022.https://heart.bmj.com/content/early/2022/08/17/heartjnl-2022-321348
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ART#
142
#微血管#
112
#主动脉#
190
#HEART#
179