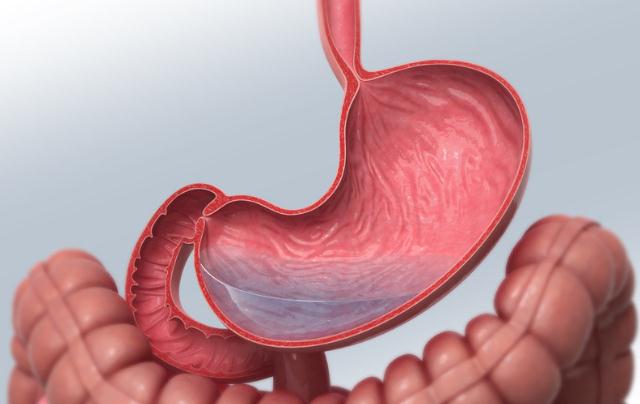
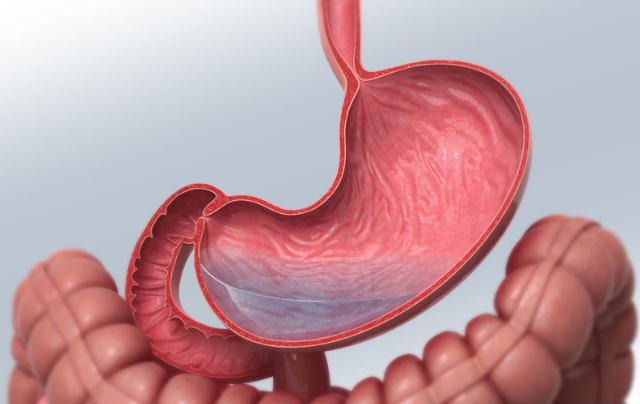
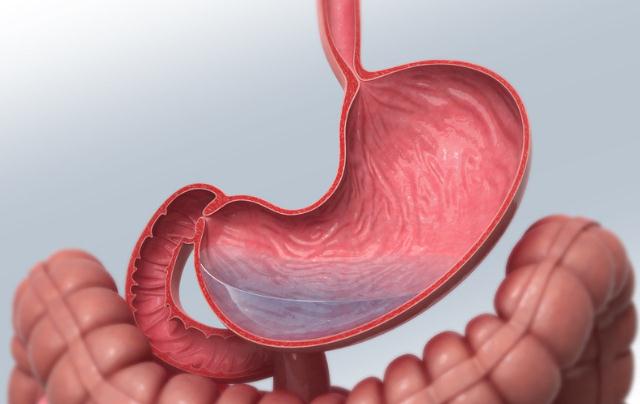
2016 NCCN临床实践指南:胃癌-证据块(2016. V3)
2016-11-28 美国国家综合癌症网络(NCCN,National Comprehensive Cancer Network) NCCN官网
2016年8月,美国国家综合癌症网络(NCCN)发布了胃癌指南2016年第3版证据块。全文获取:下载地址:指南下载(需要扣积分2分, 梅斯医学APP免积分下载)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#实践指南#
25
很好 学习
52
很好,不错,以后会多学习
51
#NCCN#
26
#临床实践#
32
#临床实践指南#
25
讲的好,学习了
51