Fundamental Research:贺静团队综述神经母细胞瘤液体活检研究进展
2022-08-27 “生物世界”公众号 “生物世界”公众号
针对NB生物学特性的新疗法对于NB的个体化治疗具有重要的临床价值。然而,目前NB的生物标志物主要通过组织活检进行分析。近年来,基于液体活检的NB循环生物标志物越来越受到关注。
近日,广州市妇女儿童医疗中心儿科研究所外科实验室贺静课题组在国家自然科学基金委员会主管、主办的高起点、高水平综合期刊 Fundamental Research 上发表了题为:Advances in liquid biopsy in neuroblastoma 的综述论文。

广州市妇女儿童医疗中心儿研所贺静研究员为通讯作者,北京大学深圳研究生院卓振健博士后和广州医科大学附属广州市妇女儿童医疗中心林磊研究生并列第一作者,儿研所缪蕾副研究员和李猛博士后为贡献作者。
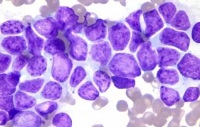
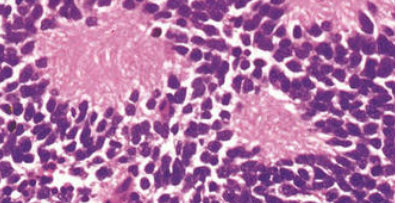
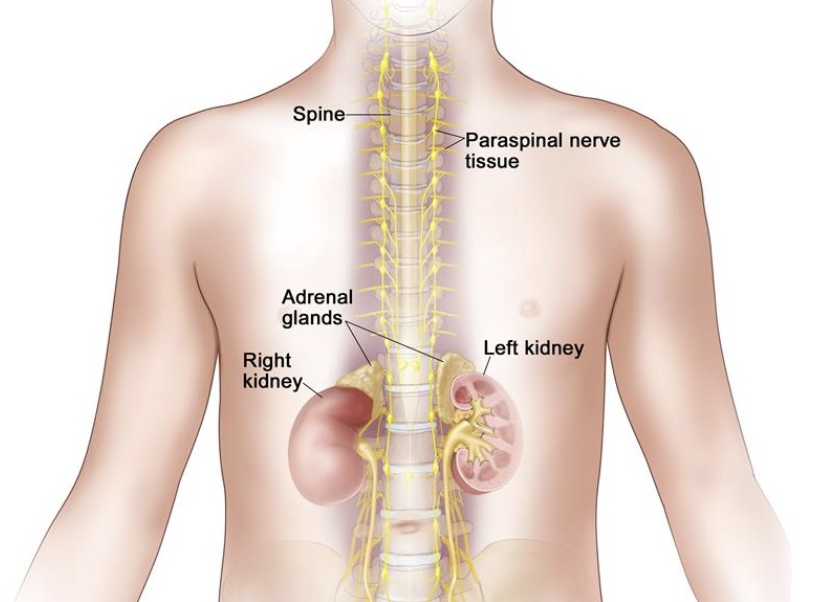
即使对高危神经母细胞瘤(NB)患者进行强化治疗,仍有一半的高危NB患者复发。针对NB生物学特性的新疗法对于NB的个体化治疗具有重要的临床价值。然而,目前NB的生物标志物主要通过组织活检进行分析。近年来,基于液体活检的NB循环生物标志物越来越受到关注。
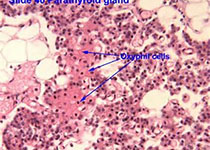
液体活检有着相对于组织活检而言的侵入性小的优势。在NB中,循环肿瘤细胞(CTC)、循环肿瘤 DNA(ctDNA)、循环DNA(cfDNA)、循环RNA(cfRNA)、核小体和外泌体等常见的液体活检分析物存在着具有重要临床意义的生物学改变。
目前检测这些液体活检分析物的技术的不断发展也为液体活检在NB肿瘤研究中的应用提供了越来越可靠的技术支持。也已经有越来越多的实验揭示了液体活检的生物标志物的很好的肿瘤特异性。随着液体活检循环生物标志物的检测技术的不断发展和肿瘤特异性的不断验证,液体活检在NB中的诊断、预后、监测疾病进展和微小残留疾病的临床应用相信很快迎来曙光。

贺静团队主要工作聚焦在儿童肿瘤的分子流行病学及机制研究,其课题组近期发表了系列相关研究,包括:
(1)发现BER通路FEN1基因rs174538多态性改变可显着降低神经细胞瘤发病风险(Cancer Communications);
(2)发现NER通路XPC基因具有作为肝母细胞瘤发病风险的生物标记物潜力(International Journal of Cancer);
(3)发现肿瘤相关巨噬细胞中的FABP4通过泛素化ATPB抑制NF-κB-IL1α通路,促进神经母细胞瘤进展(Clinical and Translational Medicine);
(4)发表靶向RAS治疗神经母细胞瘤最新科学进展(Pharmacology & Therapeutics);
(5)发表METTL14基因在肿瘤中的作用及机制最新科学进展(Journal of Hematology & Oncology);
(6)发表m6A修饰在儿童肿瘤中的作用及机制最新科学进展(BBA - Reviews on Cancer);
(7)发表m7G修饰对癌症的作用(Trends in Cell Biology)。
广州市妇女儿童医疗中心贺静团队常年欢迎生命科学、统计学及医学类博士后、研究生等有志之士加入,共创未来。
有意向者可以发邮件至editor@bioon.com联系交流。
参考文献:
1. Zhenjian Zhuo#, Chunlei Zhou#, Yuan Fang#, Jinhong Zhu, Hongting Lu, Haixia Zhou, Haiyan Wu, Yizhen Wang*, Jing He*: Correlation between the genetic variants of base excision repair (BER) pathway genes and neuroblastoma susceptibility in eastern Chinese children. Cancer Communications 2020, 40: 641-646.
2. Zhenjian Zhuo#, Lei Miao#, Wenfeng Hua#, Huitong Chen, Zhonghua Yang, Yong Li, Jiao Zhang, Suhong Li, Jiwen Cheng, Li Li, Huimin Xia, Jing He*: Genetic variations in nucleotide excision repair pathway genes and hepatoblastoma susceptibility. International Journal of Cancer 2021, 149(9):1649-1658.
3. Lei Miao#, Zhenjian Zhuo#, Jue Tang#, Xiaomei Huang, Jiabin Liu, Haiyun Wang, Huimin Xia*, Jing He*: FABP4 deactivates NF-κB-IL1α pathway by ubiquitinating ATPB in tumor-associated macrophages and promotes neuroblastoma progression. Clinical and Translational Medicine 2021, 11(4):e395.
4. Lei Lin#, Lei Miao#, Huiran Lin, Jiwen Cheng, Meng Li, Zhenjian Zhuo*, Jing He*: Targeting RAS in neuroblastoma: Is it possible? Pharmacology & Therapeutics 2021, 236:108054.
5. Qian Guan#, Huiran Lin#, Lei Miao#, Huiqin Guo, Yongping Chen, Zhenjian Zhuo*,Jing He*: Functions, mechanisms, and therapeutic implications of METTL14 in human cancer. Journal of Hematology & Oncology 2022, 15:13.
6. Yongping Chen#, Lei Miao#, Huiran Lin#, Zhenjian Zhuo*, Jing He*: The role of m6A modification in pediatric cancer. Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.
7. YongpingChen#, HuiranLin#*, LeiMiao, JingHe*:Role of N7-methylguanosine (m7G) in cancer. Trends Cell Biol 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#母细胞瘤#
66
#Mental#
40
#活检#
73
#研究进展#
53
#细胞瘤#
53
#Research#
32
#NDA#
38
内容非常好
53