Cell Res:钱友存等抗感染免疫研究获进展
2012-05-19 上海生科院健康所 上海生科院健康所
4月10日,国际著名杂志Cell Research在线发表中科院上海生命科学研究院/上海交通大学医学院健康科学研究所钱友存研究组关于NLRC5在抗胞内菌感染过程中的作用研究成果“NLRC5 regulates MHC class I antigen presentation in host defense against intracellular pathogens,”。 真核生物的天然免疫
4月10日,国际著名杂志Cell Research在线发表中科院上海生命科学研究院/上海交通大学医学院健康科学研究所钱友存研究组关于NLRC5在抗胞内菌感染过程中的作用研究成果“NLRC5 regulates MHC class I antigen presentation in host defense against intracellular pathogens,”。
真核生物的天然免疫是抵抗外界病原体入侵的第一道防线。天然免疫主要是通过模式识别受体来识别病毒或细菌等外来病原体。Nod样受体(NLR)是近年来研究发现的识别胞内菌的模式受体。NLRC5作为Nod样受体家族中最大的一个成员,其生理学功能一直不清楚。
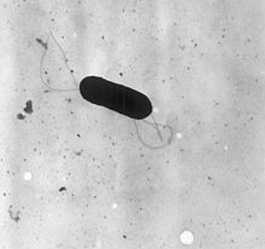
该工作主要由博士生姚依昆和王亚龙在钱友存研究员的指导下完成。该论文首次利用NLRC5基因敲除小鼠研究发现NLRC5在宿主抵抗胞内菌感染方面发挥重要作用。NLRC5通过调控I类主要组织相容性复合体(MHC class I)的转录表达,进而影响胞内病原菌(李斯特菌,L. monocytogenes)特异性CD8+ T细胞的激活和增殖,从而有效清除病原菌。该研究阐明了宿主抗胞内菌感染的新机制,为感染性疾病的预防与治疗提供了重要的理论基础。
该课题获得国家自然科学基金委、国家科技部、中国科学院和上海市科委等经费资助。(生物谷Bioon.com)

doi:10.1038/cr.2012.56
PMC:
PMID:
NLRC5 regulates MHC class I antigen presentation in host defense against intracellular pathogens
Yikun Yao1,*, Yalong Wang1,*, Fuxiang Chen2, Yin Huang1, Shu Zhu1, Qibin Leng3, Hongyan Wang4, Yufang Shi1 and Youcun Qian1
NOD-like receptors (NLRs) are a family of intracellular proteins that play critical roles in innate immunity against microbial infection. NLRC5, the largest member of the NLR family, has recently attracted much attention. However, in vitro studies have reported inconsistent results about the roles of NLRC5 in host defense and in regulating immune signaling pathways. The in vivo function of NLRC5 remains unknown. Here, we report that NLRC5 is a critical regulator of host defense against intracellular pathogens in vivo. NLRC5 was specifically required for the expression of genes involved in MHC class I antigen presentation. NLRC5-deficient mice showed a profound defect in the expression of MHC class I genes and a concomitant failure to activate L. monocytogenes-specific CD8+ T cell responses, including activation, proliferation and cytotoxicity, and the mutant mice were more susceptible to the pathogen infection. NLRP3-mediated inflammasome activation was also partially impaired in NLRC5-deficient mice. However, NLRC5 was dispensable for pathogen-induced expression of NF-κB-dependent pro-inflammatory genes as well as type I interferon genes. Thus, NLRC5 critically regulates MHC class I antigen presentation to control intracellular pathogen infection.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#钱友存#
29
#Cell#
23
#CEL#
22
#研究获进展#
52