TCR-T——CAR-T细胞治疗后新一代抗肿瘤利器
2019-08-06 不详 网络
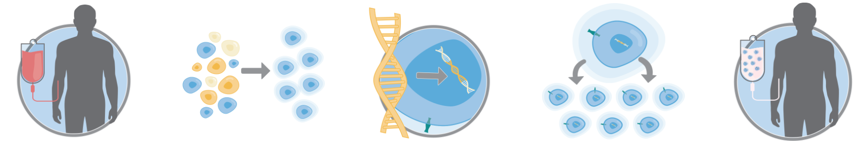
1、TCR-T是什么? T细胞受体工程化T细胞(T-cell receptor engineered T cells,TCR-T)治疗是一种新型的过继细胞治疗方法,主要是利用基因编辑技术,将能特异性识别肿瘤抗原的T细胞受体(T-cell receptor,TCR)基因导入患者T细胞内,使其表达外源性TCR,从而具有特异性杀伤肿瘤细胞的活性。 TCR-T治疗过程 来
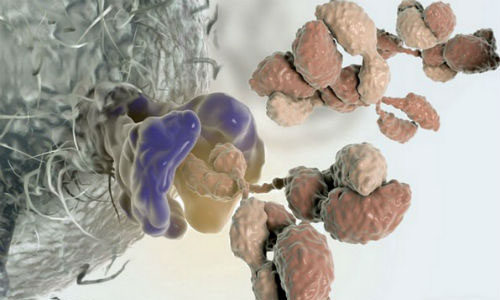
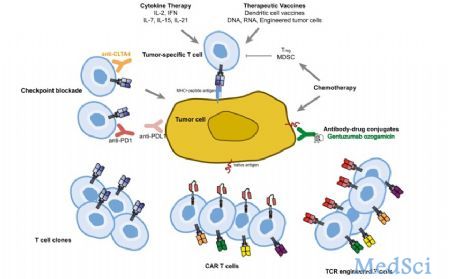
1、TCR-T是什么? T细胞受体工程化T细胞(T-cell receptor engineered T cells,TCR-T)治疗是一种新型的过继细胞治疗方法,主要是利用基因编辑技术,将能特异性识别肿瘤抗原的T细胞受体(T-cell receptor,TCR)基因导入患者T细胞内,使其表达外源性TCR,从而具有特异性杀伤肿瘤细胞的活性。 TCR-T治疗过程 来源:Kite官网 2002年,ROSENBERG团队率先发现:从黑色素瘤中分离出的肿瘤浸润淋巴细胞(Tumor infiltrating lymphocyte,TIL)经体外扩增回输后,可以特异性杀伤肿瘤细胞。但是在其他肿瘤中,TIL往往不易获取且体外扩增时间长,扩增后多为终末分化的T细胞,持续抗肿瘤效果较弱。在这样的背景下,人们探究能否在正常外周血淋巴细胞(Peripheral blood lymphocyte,PBL)上导入已知的抗原特异性TCR基因进行治疗,这便是TCR-T细胞治疗的由来。 Morgan等人2006年在Science上发表的一篇文章显示,经基因修饰的TCR-T细胞在黑色素瘤的治疗中显示了较好的应用前景(
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CAR-#
31
#TCR-T#
46
#TCR#
32
向科研人员致敬!!!
78