Nat Commun:黑色素瘤耐药机制研究取得突破性进展
2018-03-10 佚名 西安交通大学
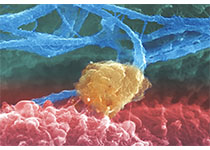
近日,西安交大生命学院线粒体生物医学研究所和前沿院转化医学研究中心等单位合作,发现了一种新的基于磷酸化与SUMO化修饰的SOX10转录活性调控机制,揭示了ERK1/2/SOX10/FOXD3/ERBB3信号通路在人黑色素瘤对RAF抑制剂的适应性耐药发生过程中的作用。这一突破性的进展将会极大地促进以SOX10为靶点提高黑色素瘤的治疗效果方面的研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#色素#
22
#COMMUN#
24
#Nat#
30
#机制研究#
21
#耐药机制#
35
很好的学习材料.对临床和科研都有很大帮助作用.水滴石穿.不断积累.
82
很好
90
#黑色素#
28
#黑色素#
25
学习了受益匪浅
84