JCO:TP53胚系突变与儿童急性淋巴细胞白血病的易感性和预后的关系
2018-01-13 佚名 肿瘤资讯
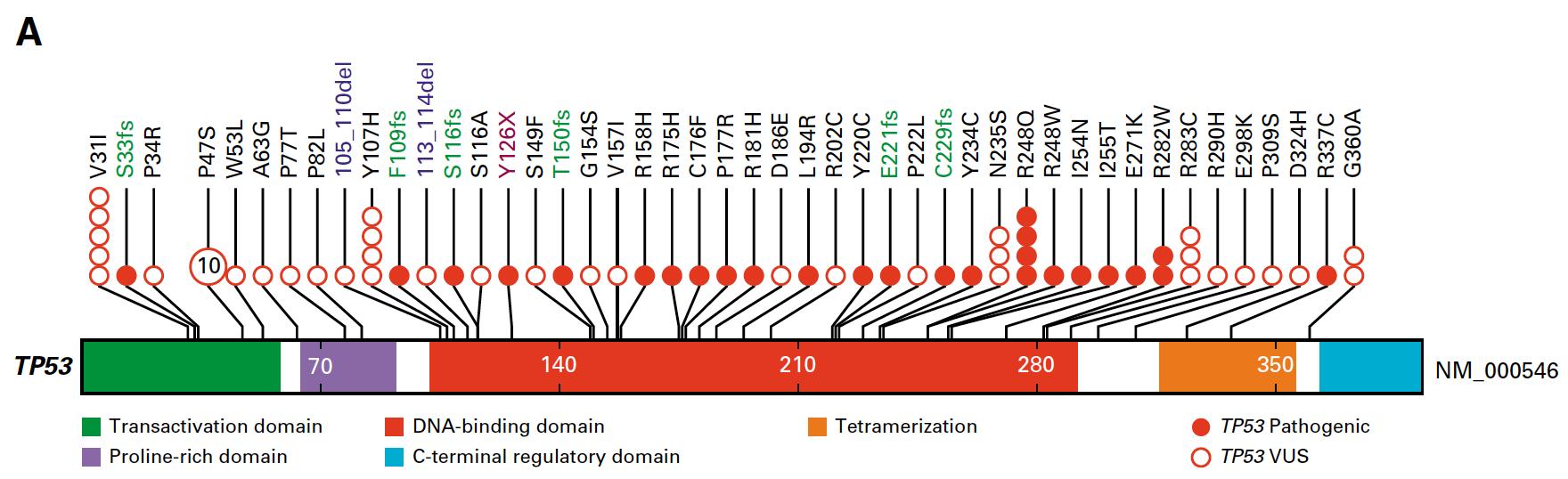
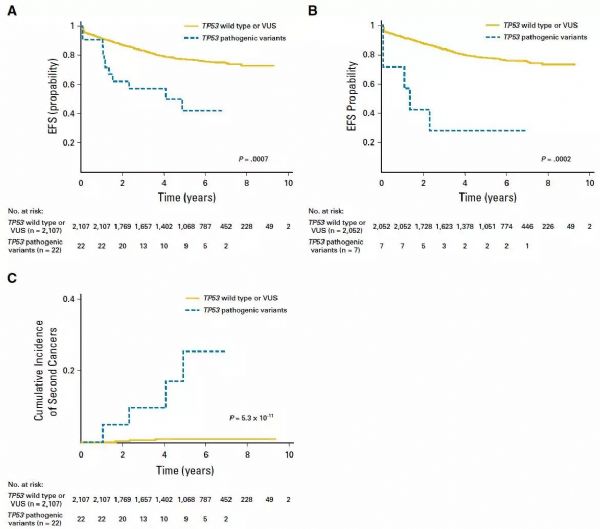
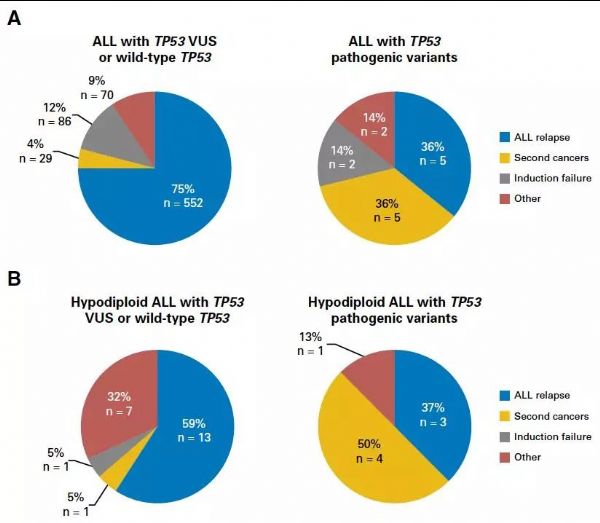
急性淋巴细胞白血病(ALL)是儿童常见的恶性肿瘤,越来越多的证据显示其与遗传易感性相关。TP53是重要的抑癌基因,在多种肿瘤中检测到TP53的突变。近日,《JCO》发表的一项研究在大样本量的儿童ALL患者检测TP53的胚系突变,并探索致病性突变与患者治疗疗效和预后的关系。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了.谢谢
60
#淋巴细胞白血病#
40
#JCO#
40
学习了.谢谢分享
67
学习了.谢谢分享
70
学习了.谢谢分享
52
#淋巴细胞#
27
#p53#
37
#TP53#
50
#易感性#
0