Eur J Prev Cardiol:面对CKD和HFpEF双重打击 RASI带来生的希望
2018-09-28 吴星 环球医学网
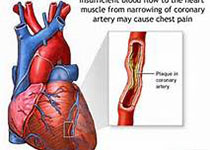
射血分数保留型心衰(HFpEF)是一种临床综合征,患者表现出心衰的体征和症状,但左心室射血分数仍正常或接近正常。约一半的心衰患者射血分数保留,并且这一比例一直在增加。肾素-血管紧张素系统抑制剂(RASI)是慢性肾病(CKD)的一线疗法,但是此类药物能否改善合并CKD的射血分数保留型心衰(HFpEF)患者的结局,仍是未知。
日本学者在《Eur J Prev Cardiol》发表一项研究,考察了RASI治疗轻度至中度CKD合并HFpEF患者的有效性。
这是醛固酮拮抗剂治疗心脏功能保留型心衰试验的事后分析。
总共1465名合并轻度至中度CKD的HFpEF患者入组。平均随访2.8年;502名患者出现了至少1个经证实的首要结局事件。未服用和服用RASI患者的首要结局事件发生率分别为175.4和112.8/1000人-年。服用RASI的患者首要结局事件和全因死亡风险显着低于未服用患者。倾向得分匹配患者中,服用RASI的患者的这些风险显着低于未服用患者。
本研究显示,在伴有轻度至中度CKD的HFpEF患者中,服用RASI的患者主要结局事件和全因死亡的风险显着低于未服用RASI的患者。未观察到RASI使用与糖尿病之间显着的相互作用。此外,在倾向评分匹配分析中,主要结局的差异依然显着。
RASI可降低CKD患者终末期肾病、心血管事件和全因死亡的风险。因为RASI具有特定的肾保护获益,很多临床实践指南,包括肾病改善全球结局指南,推荐RASI作为CKD患者的一线治疗,特别是蛋白尿患者。很多大规模临床试验还证实,心力衰竭患者应用ACEI可以明显改善远期预后,降低死亡率。
该研究则进一步证实,合并轻至中度CKD的HFpEF患者中,RASI的使用与不良心血管结局风险降低相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cardiol#
36
#RASI#
39
#PE#
27
#HFpEF#
47