SLIPA喉罩全身麻醉期间误吸致肺不张一例
2019-11-15 唐苗苗 罗云 柏科莉 华西医学
患者,男,13岁,身高165 cm,体重58kg。因“左下肢先天性血管畸形伴溃疡”于2017年11月4日入院,拟择期全身麻醉下行“左下肢血管介入栓塞术”。术前病史、体格检查(查体)、辅助检查均无特殊。
1.病例介绍
患者,男,13岁,身高165 cm,体重58kg。因“左下肢先天性血管畸形伴溃疡”于2017年11月4日入院,拟择期全身麻醉下行“左下肢血管介入栓塞术”。术前病史、体格检查(查体)、辅助检查均无特殊。
入室后常规核对患者信息并确认禁饮禁食时间已经超过8h,监测脉搏氧饱和度(pulse oxygen saturation,SpO2)、无创动脉血压、心电图,建立静脉通道后开始麻醉诱导:静脉注射咪达唑仑注射液2mg、枸橼酸舒芬太尼20μg、注射用顺苯磺酸阿曲库铵9mg、丙泊酚注射液90mg4min后,插入49#SLIPATM(the Stream lined Liner of the Pharynx Airway)喉罩。置入喉罩后可见口腔内溢出约20mL清亮液体,充分吸引后静脉注射盐酸戊乙奎醚注射液0.4mg,使用麻醉机压力控制模式通气,参数设置为:吸入气氧浓度(fractional concentration of inspired oxygen,FiO2)50%,呼吸频率12次/min,气道压力12 cmH2O(1 cmH2O=0.098kPa),吸呼比1:2,潮气量400mL。吸入2%七氟烷,辅以盐酸右美托咪定注射液持续泵注维持麻醉。
手术开始前摆放左侧躯体稍垫高体位后,气道压力突然增高至25 cmH2O、潮气量仅250mL,立即调整喉罩位置但通气效果无改善,并且气道压力继续增高至30 cmH2O、潮气量降至150mL,SpO2从100%进行性降至75%。立即拔出喉罩,改气管插管。插管过程见罩体空腔及患者口腔内又溢出清亮液体约25mL。充分吸引后予6L/min纯氧面罩手控通气,阻力较大。呼吸机使用压力模式控制通气,限压35 cmH2O,频率12次/min,潮气量仍只有200mL。SpO2逐渐回升至83%,呼气末二氧化碳分压(partial pressure of end-tidal carbon dioxide,PetCO2)60mmHg(1mmHg=0.133kPa)。
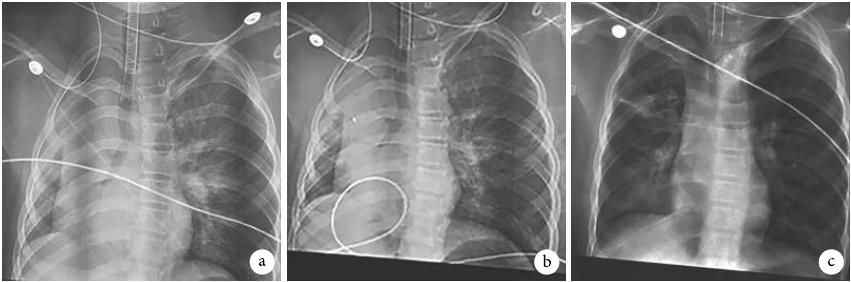
查体:患者右侧胸壁塌陷,机械通气动度明显减弱,肋间隙变窄;叩诊右肺呈浊音;听诊左肺呼吸音稍减弱,右肺呈管样呼吸音及干鸣。X线胸部透视显示右侧全肺变小,透光度下降,气管和心脏移向右侧(图1a)。纤维支气管镜检查左肺无异常,右肺未见异物及黏稠分泌物,仅吸出少量清亮液体。综合考虑为右肺不张、低氧血症。处理方法:①生理盐水右肺灌洗;②注射用甲泼尼龙琥珀酸钠80mg、呋塞米5mg静脉注射;③用麻醉机实施手法肺复张3次;④呼吸机机械通气增加呼气末正压(positive end-expiratory pressure,PEEP)至12 cmH2O。10min后,通气情况有所改善,SpO2上升至92%,肺顺应性好转,气道压力逐渐下降,潮气量增加,PetCO2降至55mmHg。但再次X线胸部透视示:右肺未复张(图1b)。将气管导管在纤维支气管镜引导下插入右侧主支气管内,使用30 cmH2O压力持续30s连续实施手法肺复张3次。5min后X线胸部透视:右肺透光明显好转,右肺已复张(图1c)。且SpO2立即上升至95%,气道压力逐步下降至20 cmH2O,潮气量上升至350mL,PetCO2逐步下降至正常。暂时取消手术,继续进行呼吸机支持治疗4h。患者自主呼吸恢复,转麻醉恢复室,完全清醒后顺利拔除气管导管,安返病房。该患者2周后,分别在气管插管和喉罩全身麻醉下各实施手术1次,均无特殊,1个月后康复出院。
图1 患者胸部X线片图像a.气管内插管后即刻,可见右侧肺不张,并伴有右侧肋间隙变窄,气管、纵隔向右侧移位,右侧膈肌抬高,左肺代偿性肺气肿;b.经纤维支气管镜冲洗及吸引、手法肺复张、PEEP正压通气等综合措施治疗后,可见右侧肺未复张;c.经单侧支气管插管、正压手法肺复张后,可见右侧肺已复张
2.讨论
使用喉罩实施全身麻醉,已经普遍成为短小手术常用的一种通气管理方式。SLIPATM喉罩是一款根据解剖结构预塑形、免充气声门上通气装置,在国内外、尤其我国许多大型医疗中心应用广泛。虽然罩体内已设计一个可容纳液体的空腔,理论上可最大程度防止反流误吸,但此类喉罩外形固定且质地坚硬,喉罩型号选择不当或(和)麻醉期间罩体移位等情况均可严重影响其气道隔离密闭效果,因此SLIPATM喉罩全身麻醉期间反流误吸时有发生。此例SLIPATM喉罩全身麻醉期间发生口咽部分泌物误吸致急性右肺不张合并低氧血症的患者置入SLIPATM喉罩全身麻醉后出现低氧血症和高碳酸血症。经临床表现、胸部X线片及纤维支气管镜检查,诊断反流误吸致急性肺不张(吸入性肺不张)明确。经纤维支气管镜冲洗及吸引、手法肺复张、PEEP正压通气等综合措施治疗,效果欠佳。后经单侧支气管插管、正压肺复张,治疗效果满意。
使用喉罩全身麻醉下食道括约肌的压力下降达15%,增加了胃食道反流的风险,第一代喉罩误吸发生率约为0.02%。本例患者口咽部存在大量分泌物,在操作过程移动体位,导致分泌物沿喉罩与声门间空隙随呼吸气流误吸进入气道,随重力流入右侧主支气管及其分支,发生非固态物质微量误吸,阻塞右侧肺全部支气管系统,造成急性右肺不张和低氧血症。目前,国内外关于喉罩引起非固态物质微量吸入致急性肺不张的病例报道十分罕见。
本例患者处理棘手之处在于:拔出SLIPATM喉罩行气管插管正压通气,仍然无法使萎陷侧肺复张,无法保证满意的通气及氧合。理论上正常人拥有约86%的肺储备功能,因此单靠一侧肺通气也能维持正常氧合,然而本例患者单靠一侧肺通气氧合难以维持,其原因主要有以下2个方面:①右侧肺持续存在较多的血流;②左侧肺通气相对不足。
对应病理生理学机制如下:①本例患者左侧胸高于右侧,右肺受重力因素影响持续存在较多血流;②反流误吸引发的炎症反应导致右肺低氧性肺血管收缩功能一定程度受损。双侧通气手法肺复张无效,可能因为左肺与右肺同时接受正压时,左肺顺应性较好,减弱了对右肺的膨胀作用。
对于这种情况,果断将气管导管送入患侧(右侧)针对性进行右肺加压通气,既可防止通气压力过高对左肺造成损伤,又可局部增加右肺压力,是一种简单有效的治疗措施。通过本例患者的治疗抢救,我们认为使用喉罩(尤其是免充气喉罩,如SLIPATM)进行较长时间机械通气时,应当注意以下几点:
①虽然喉罩对气道刺激轻微、麻醉深度要求较低,可用于保留自主呼吸时的辅助通气,但是自主呼吸时咽喉部肌肉张力增加以及难以避免的吞咽反射均可能导致喉罩移位,因此喉罩最优通气模式为压力控制通气,另外必须注意的是,以SLIPATM喉罩为代表的硬质预定型喉罩的最佳通气体位为平卧位或头高脚低仰卧位,因此在使用喉罩实施机械通气时必须严格掌握其适应证与禁忌证;②术中密切监测通气情况,及早发现反流误吸的发生;③若怀疑已发生反流误吸,应及时查体并听诊双肺呼吸音;④尽早使用纤维支气管镜检查气道内情况,排除异物阻塞气道可能,并辅助诊断;⑤尽早行胸部X线检查确诊;⑥及时将喉罩更换为气管内插管,保障有效通气和呼吸治疗,如手法肺复张;⑦早期采取综合治疗措施,如充分吸引,吸氧,加用PEEP,静脉注射糖皮质激素,必要时支气管灌洗;⑧可及早使用患侧支气管插管进行患侧手法肺复张;⑨当肺复张后,进行2~4h的呼吸支持治疗很有必要。
总之,使用喉罩全身麻醉,应高度重视反流误吸所致的肺不张,麻醉前使用减少呼吸道分泌物的药物,严密观察,早发现早治疗低氧血症尤为重要。
原始出处:
唐苗苗,罗云,柏科莉,王晓,周棱,刘斌.SLIPA~(TM)喉罩全身麻醉期间误吸致肺不张一例[J].华西医学,2018,33(12):1577-1578.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








精彩病例
73
#SLIPA喉罩#
39
#肺不张#
52
非常精彩,受益非浅
88
病例非常精彩
95