Eur Respir J:低风险肺栓塞患者右室扩张的预后价值!
2017-12-17 xing.T MedSci原创
由此可见,在sPESI为0的患者中,MDCT检查时RV/LV≥0.9和≥1.0较为常见,但与预后较差无关,这些患者中,较高的截止值可能与更加糟糕的结局相关。
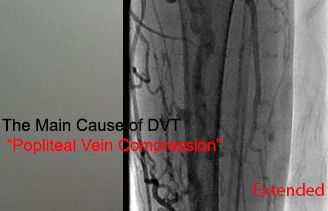
多排螺旋CT(MDCT)在评估肺栓塞(PE)患者和简化肺栓塞严重程度指数(sPESI)为0的患者右心室扩张(RVD)中的预后价值尚不清楚。近日,呼吸疾病领域权威杂志Eur Respir J上发表了一篇研究析文章,研究人员探究了这些患者MDCT评估的RVD,由右心室与左心室比值来(RV/LV)≥0.9或≥1.0来定义,是否与不良预后相关。
研究人员结合了三个前瞻性队列研究的数据。该研究的主要结局为sPESI为0的患者30天的全因死亡、血流动力学崩溃或复发性PE。
在779例sPESI为0的患者中,分别有420例(54%)和299例(38%)患者RV/LV≥0.9和≥1.0。在主要研究终点之间研究人员未观察到显著差异,RV/LV≥0.9和≥1.0的患者分别为0.95%(95%可信区间为0.31-2.59) vs. 0.56%(95%可信区间为0.10-2.22;P=0.692)和1.34%(95%可信区间为0.43-3.62)和0.42%(95%可信区间为0.07-1.67;P=0.211)。将RV/LV的阈值增加至≥1.1,在RVD患者中结局发生更为常见(2.12%,95%可信区间为0.68-5.68 vs. 0.34%,95%可信区间为0.06-1.36;P=0.033)。
由此可见,在sPESI为0的患者中,MDCT检查时RV/LV≥0.9和≥1.0较为常见,但与预后较差无关,这些患者中,较高的截止值可能与更加糟糕的结局相关。
原始出处:
Benoit Côté,et al. Prognostic value of right ventricular dilatation in patients with low-risk pulmonary embolism. Eur Respir J. http://erj.ersjournals.com/content/50/6/1701611
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#扩张#
31
#预后价值#
38
谢谢.学习了
54
非常好的文章.学习了
60