JACC:经导管主动脉瓣置入术后感染性心内膜炎的手术治疗
2022-03-11 Nebula MedSci原创
心脏手术不能降低导管主动脉瓣置入术后感染性心内膜炎患者的住院死亡率和一年全因死亡率
经导管主动脉瓣置入术 (TAVI) 后感染性心内膜炎 (IE) 的发生率波动在0.7%-3.4%/人·年,与开胸主动脉瓣置换术后的IE发生率相似。TAVI-IE与住院死亡率升高相关,且患者初发IE后的存活预后较差。但是,迄今为止,TAVI-IE的最佳治疗方法仍不确定。
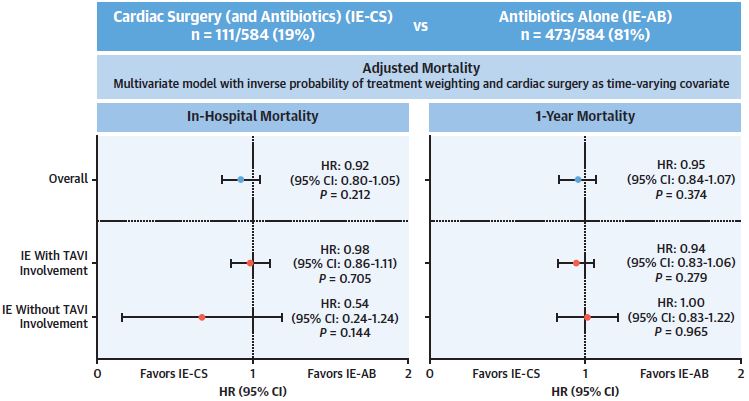
本研究目的是评估采用心脏手术联合抗生素 (IE-CS) 治疗的TAVI-IE患者的临床特点和结果,并与单使用抗生素 (IE-AB) 治疗的患者进行比较。
根据改良的Duke标准前瞻性和回顾性地从多个医疗中心纳入确定有TAVI-IE的患者(无论其心脏结构是否受影响)。基于接受的治疗方案,把所有受试患者分成两组,即心脏手术联合抗生素治疗组和单使用抗生素组。采用粗概率和治疗加权逆概率分析心脏手术和药物治疗对两组患者一年全因死亡率的影响。
采用两种治疗的患者的生存预后
共纳入了584位患者,其中111位(19%)采用了心脏手术联合抗生素治疗,473位(81%)只采用了抗生素治疗。与单使用抗生素相比,心脏手术联合抗生素并不能降低住院死亡率(HR 0.85)和一年全因死亡率(HR 0.88)。根据混杂因素偏倚校正后,心脏手术联合抗生素与单使用抗生素相比仍不能降低患者的住院死亡率(HR 0.92)和一年全因死亡率(HR 0.95)。
住院死亡率和一年全因死亡率的预测因素有EuroSCORE I、金黄色葡萄球菌感染、急性肾衰竭、持续性菌血症和脓毒症性休克。
在该研究中,大部分TAVI-IE患者只接受抗生素治疗。心脏手术虽不能降低住院死亡率和一年全因死亡率,但也与住院死亡率和一年全因死亡率升高无关。TAVI-IE患者的高死亡率更多的是与患者的特征、病原学和感染性心内膜炎相关并发症有关。
原始出处:
Mangner Norman,Val David Del,Abdel-Wahab Mohamed et al. Surgical Treatment of Patients With Infective Endocarditis After Transcatheter Aortic Valve Implantation.[J] .J Am Coll Cardiol, 2022, 79: 772-785. https://doi.org/10.1016/j.jacc.2021.11.056
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#内膜#
51
#置入术#
52
#JACC#
53
#感染性#
61
#手术治疗#
61
#ACC#
0
#主动脉瓣#
46
#心内膜炎#
66
#主动脉#
44
#经导管#
48