JACC:血栓烷生成越多,死亡风险越高!
2022-06-19 MedSci原创 MedSci原创
系统性血栓烷生成是普通人群全因死亡和心血管死亡的独立风险因素,无论有无服用阿司匹林
血栓烷A2 (TXA2)是一种具有强效血小板活化和血管收缩特性的二十烷类化合物,由花生四烯酸在环氧化酶 (COX) 和下游血栓烷合酶的作用下产生的。在健康个体中,TXA2主要在血小板中生成,阿司匹林(ASA)可通过抑制COX-1抑制TXA2的生成。
但在在四分之一以上的心血管疾病(CVD)患者中,特别是氧化应激增加的患者,非血小板组织会产生大量TXA2,而标准的ASA治疗不能完全抑制TXA2的产生。持续性地血栓烷生成,是服用ASA的CVD患者的一个重要死亡风险因素。
该研究目的是确定非选定人群(无论有无使用ASA)中系统性血栓烷生成相关的死亡风险。
通过酶联免疫吸附法测定了Framingham心脏研究3044位受试者(平均66±9岁,53.8%的女性)的尿血栓烷B2代谢物 (TXB2-M) 。采用多变量模型评估TXB2-M与生存率的相关性。
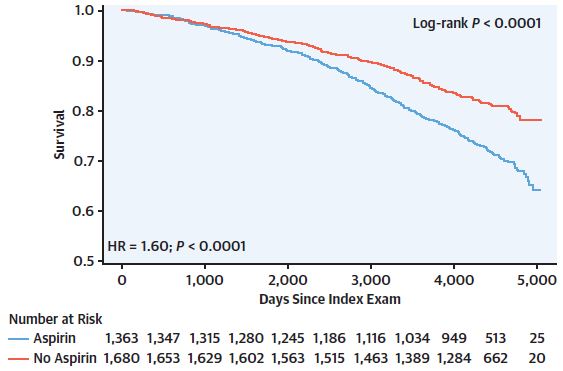
有无服用阿司匹林个体的生存率
在3044位受试者中,有1363位(44.8%)服用ASA。与非ASA服用者相比,ASA服用者的中位TXB2-M水平明显较低(1147 vs 4179 pg/mg肌酐,p<0.0001)。无论有无服用ASA,TXB2-M都与受试者的全因死亡率和心血管死亡率显著相关(HR分别是1.96和2.41,p<0.0001),而且根据相近年龄个体的死亡风险因素调整后,显著性仍存在(HR分别是1.49和1.82,p≤0.005)。
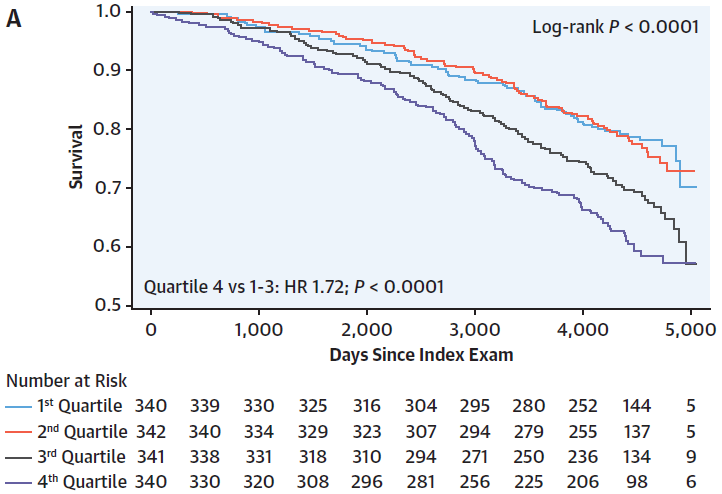
不同TXB2-M水平的阿司匹林服用者的生存率
在2353位无心血管疾病的受试者中,TXB2-M与非ASA服用者的心血管死亡率相关(校正HR 3.04),但与ASA服用者的无关;而ASA服用与低TXB2-M水平个体的全因死亡率相关,但与TXB2-M升高个体的无关。
不同TXB2-M水平的非阿司匹林服用者的生存率
简而言之,系统性血栓烷生成是普通人群全因死亡和心血管死亡的独立风险因素,无论有无服用阿司匹林;该指标的检测或可有助于调整治疗方案,特别是对于没有心血管疾病的个体。
原始出处:
Rade Jeffrey J,Barton Bruce A,Vasan Ramachandran S et al. Association of Thromboxane Generation With Survival in Aspirin Users and Nonusers.[J] .J Am Coll Cardiol, 2022, https://doi.org/10.1016/j.jacc.2022.04.034
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#JACC#
69
认真学习~~
42
#死亡风险#
49
#ACC#
57