西妥昔单抗联合化疗能使中国复发/转移性头颈部鳞癌患者获益
2018-11-30 佚名 肿瘤资讯
2018年欧洲肿瘤内科学会亚洲年会(ESMO ASIA 2018)于11月23-25日在新加坡举行。欧洲肿瘤内科学会(ESMO)成立于1975年,是欧洲领先的肿瘤内科学专业组织;2018 ESMO亚洲年会致力于使亚太地区肿瘤学专业人士与快速发展的肿瘤学科学与教育保持同步。在今年的ESMO亚洲年会上,来自上海同济大学附属东方医院的郭晔教授就复发/转移头颈鳞癌的III期CHANGE-2研究结果做了口头
郭晔主任医师,同济大学附属东方医院,肿瘤医学部副主任兼一期临床试验中心主任,中国临床肿瘤学会副秘书长,中国临床肿瘤学会头颈肿瘤专委会主委,中国临床肿瘤学会甲状腺癌专委会副主委,中国临床肿瘤学会淋巴瘤联盟常委,中国抗癌协会肿瘤化疗专业委员会青委会副主委,中国抗癌协会头颈肿瘤专业委员会委员,中国抗癌协会甲状腺癌专业委员会委员,中国抗癌协会鼻咽癌专业委员会委员,中国抗癌协会血液肿瘤专业委员会委员,中国抗癌协会淋巴瘤专业委员会委员上海市抗癌协会淋巴瘤专业委员会秘书长,上海市抗癌协会头颈肿瘤专业委员会副主委
CHANGE-2研究结果公布,中国头颈部鳞状细胞癌患者终将受益
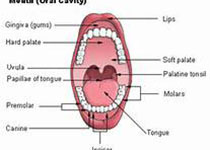
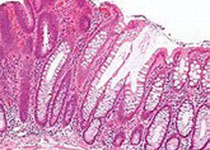
CHANGE-2研究是针对中国晚期头颈部鳞状细胞癌患者进行的一线全国多中心的三期随机对照研究。这项研究共入组243例R/M头颈部鳞癌患者,按照2:1的比例,随机接受西妥昔单抗+化疗或单纯化疗结果显示,对比单纯化疗,西妥昔单抗联合化疗能够显着的改善无进展生存期(PFS)、总生存期(OS)和缓解率(ORR)。因此这项研究与针对欧美高加索人种的EXTREME试验有相似的临床结果。由此可见,抗EGFR单抗——西妥昔单抗同样能使中国R/M头颈部鳞状细胞癌患者受益,研究的结果对于中国患者具有非常重要的意义。
CHANGE-2研究显示:西妥昔单抗治疗头颈部鳞癌安全性有保证
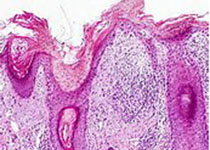
作为抗EGFR靶向药物,西妥昔单抗确实存在比较特殊的毒副反应,这不同于常规化疗药物。特殊的毒副反应包括痤疮样皮疹、输液相关不良反应等。在CHANGE-2研究中,这样的不良反应同样存在,但总体来讲这些不良反应都是1/2级不良反应,发生3/4级不良反应的人群不超过5%,很少有患者因为不良反应出现药物减量或者停药。综合看来,靶向药物西妥昔单抗的安全性非常好,与在高加索人群中进行的EXTREME研究相类似,未出现新的或意外的不良反应。药物毒性不会影响中国患者选择西妥昔单抗治疗疾病。
基于CHANGE-2研究,国内指南将与国际接轨
今年更新的NCCN指南和ESMO指南都推荐西妥昔单抗联合化疗是R/M头颈部鳞癌的一线治疗,1类证据,因为有相应的临床证据和循证医学证据支持。但是在今年颁布的CSCO头颈部肿瘤指南中,西妥昔单抗联合化疗一线治疗R/M头颈部鳞癌被列为2类证据。这是由于目前中国尚未批准西妥昔单抗用于R/M头颈部鳞癌。相信随着CHANGE-2研究的问世,明年CSCO指南的更新将会包含西妥昔单抗联合化疗治疗R/M头颈部鳞癌。最终患者将从中获益。
西妥昔单抗进入医保,更多患者受益
患者从医保获益,这显而易见。CHANGE-2研究结果显示,西妥昔单抗联合化疗,肿瘤缓解率能够翻一倍,进而延长无病生存与总生存期,使得患者获益明显。对头颈部鳞癌的患者来说,肿瘤的进展常会使患者出现吞咽障碍、疼痛等症状,所以肿瘤的缓解对患者的生活质量有非常重要的帮助。当将来通过医保覆盖,使更多患者通过国家政策用上西妥昔单抗,在患者生存获益的同时,生存质量也能进一步获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#西妥昔#
54
#鳞癌患者#
51
#转移性#
40
#联合化疗#
45
#鳞癌#
41
#头颈部#
33
#颈部#
32