腹痛反酸无特异性消化道症状 此病易误诊和漏诊
2018-11-12 冯起校 黄汉伟 专科医师培训指南---内科病例讨论
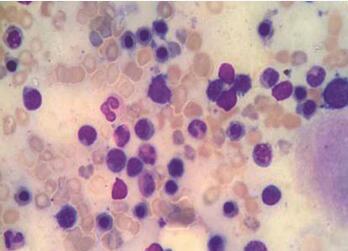
男性患者,25岁,因“口干、多饮、多尿”入院治疗。2天前无明显诱因出现纳差、上腹痛,伴反酸、嗳气、恶心、呕吐,逐渐出现全身乏力、胸闷、气促、双下肢麻木,伴咳嗽、咳痰,口干、多饮、多尿加重。既往有“慢性胃炎”病史10 余年。有“鼻中隔偏曲”病史,未行手术治疗。有嗜烟、酒史5年。患者所患何病?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#特异性#
30
学习了
81
学习了
81
#腹痛#
27
#漏诊#
21
#消化道#
25