中科院上海药物所蒋华良课题组、杨财广课题组及北京基因组所刘江课题组在一项合作研究中确证了肾癌治疗新靶点SPOP。9月12日,相关成果在线发表于《癌症细胞》杂志。
以索拉非尼和舒尼替尼为代表的靶向抗肿瘤药物是晚期肾癌的一线治疗药物,但对转移性肾癌的疗效十分有限,并且容易产生耐药。因此,当前亟待发现并确证治疗肾癌特异性药物作用新靶标。
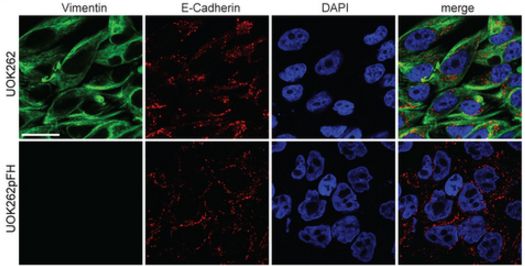
SPOP介导许多核蛋白的泛素化修饰,引发蛋白降解,从而调控细胞的多种功能。此前研究发现,SPOP是透明细胞肾癌的生物标志分子,同时低氧微环境驱使过表达的SPOP蛋白在肾癌细胞质中大量累积,最终促进肾癌形成。
此次研究人员以SPOP与蛋白质的相互作用为靶标,根据SPOP识别底物多肽的复合物晶体结构的特点,综合应用多种技术手段,获得了能与SPOP结合的小分子化合物。该化合物能抑制SPOP与底物蛋白质的结合,干预SPOP介导的调控PTEN、DUSP7等抑癌蛋白泛素化修饰的信号转导通路,最终抑制肾癌细胞的生长。
相关专家表示,该项研究为SPOP能否作为透明细胞肾癌药物靶标进行了药理功能确证,同时为SPOP抑制剂的发现并运用于治疗肾癌指明了不同于激酶抑制剂的新方向。

SPOP是特异性治疗肾癌的潜在新靶点
原始出处
Zhong-Qiang Guo12, Tong Zheng12, Baoen Chen12, Cheng Luo12, Sisheng Ouyang12, Shouzhe Gong, Jiafei Li, Liu-Liang Mao, Fulin Lian, Yong Yang, Yue Huang, Li Li.et.al.Small-Molecule Targeting of E3 Ligase Adaptor SPOP in Kidney Cancer.Cancer cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
38
#cancer cell#
29
#中科院#
35
#CEL#
38
#上海药物所#
41
#新靶点#
28
#治疗新靶点#
25