Respirology:胸腔积液肺癌患者的临床特征和存活率
2015-02-24 范伟 MedSci原创
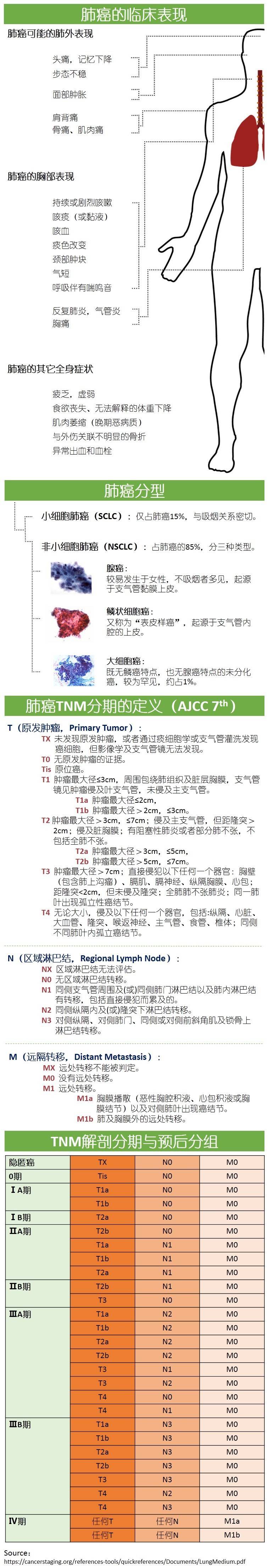
背景和目的:胸腔积液肺癌的临床意义很少进行系统性的梳理。本研究的目的是确定肺癌合并胸腔积液患者的患病率,病因和自然历史,以及对他们生存的影响。方法:在我们机构中,对新诊断的超过4年的556例肺癌患者的影像学和临床资料进行回顾分析。结果:肺癌患者包括490例非小细胞肺癌和66例小细胞类型的肺癌。约40%的肺癌患者在他们的疾病过程中伴有胸腔积液。有一半的患者胸腔积液太小可吸取掉。这些积液没有发展到需要
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺癌患者#
29
#存活率#
24
#临床特征#
26
很不错学习了
110
不错的文章,学习了
120
明白了
60
确实,临床见
105
速度~
148