Lancet Neurol:急性缺血性卒中可早期应用阿替普酶治疗
2016-06-18 MedSci MedSci原创
背景:随机试验表明,急性缺血性卒中患者4.5h内应用阿替普酶,可增加良好预后的的可能。然而,阿替普酶也增加脑出血的风险;研究者旨在确定不同类型患者,应用阿替普酶对脑出血,死亡率和功能损害风险的比例和绝对的影响。方法:研究者使用卒中溶栓试验(STT)中,阿替普酶与安慰剂或空白对照的随机试验的荟萃分析中,获取急性缺血性脑卒中患者的数据。研究这将脑出血预先分为三类:7天内2型脑实质出血;24-36 h出
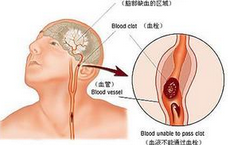
背景:随机试验表明,急性缺血性卒中患者4.5h内应用阿替普酶,可增加良好预后的的可能。然而,阿替普酶也增加脑出血的风险;研究者旨在确定不同类型患者,应用阿替普酶对脑出血,死亡率和功能损害风险的比例和绝对的影响。
方法:研究者使用卒中溶栓试验(STT)中,阿替普酶与安慰剂或空白对照的随机试验的荟萃分析中,获取急性缺血性脑卒中患者的数据。研究这将脑出血预先分为三类:7天内2型脑实质出血;24-36 h出血在(SITS-MOST)(2型脑实质出血, NIHSS 评分恶化4分);7天致死性脑出血。研究者用logistic回归分析,通过试验分层,对阿替普酶治疗,延迟治疗,年龄剂卒中严重程度,构建脑出血概率的对数模型。研究者做了探索性的分析,评估脑出血后死亡率,并且检测脑出血的绝对风险。
结果:共纳入9个静脉注射阿替普酶VS 对照组的试验,6756名受试者。阿替普酶可增加2型脑实质出血(231 [6.8% ] /3391例阿替普酶vs 44 (1 .3%)/ 3365例对照组; OR 5.55 [ 95% CI 4.01-7.70 ];绝对增加5.5% [ 4.6-6.4 ]);SITS-MOST出血(124 [3.7% ]/ 3391 vs 19 [0.6% ]/3365;OR 6.67 [ 4.11-10.84 ];绝对增加3.1% [ 2.4-3.8 ])和致死性脑出血(91 [ 2.7% ] /3391 vs 13 [0.4% ]/3365;OR 7.14 [ 3.98-12.79 ];绝对增加2.3% [ 1.7-2.9 ])的几率。无论如何定义,不管是否延迟治疗,年龄及基线卒中的严重程度,脑出血的比例增加是相似的,但随着卒中严重程度的增加,颅内出血的绝对风险增加:对于SITS-MOST脑出血,NIHSS评分0-4到22或更高,绝对风险范围从1.5%(0.8-2.6%)到3.7%(2.1-6.3%)。在4.5h内处理的患者,获得良好预后(mRS:0或1)的比率增加(6.8% [ 4.0%到9.5% ]),超过致死性脑出血绝对风险的增加(2.2% [ 1.5%到3.0% ])和任何90天内死亡风险的增加(0.9% [ 1.4%到3.2% ])。
解释:给予阿替普酶患者中,净预后是开始治疗的时间(治疗越快,良好预后的比例增加)和卒中的严重程度(卒中越严重,脑出血的绝对风险增加)来预测的。4.5小时内阿替普酶治疗获得良好预后的概率超过死亡的风险,早期治疗对重症脑卒中患者尤其重要。
原始出处:
Whiteley WN, Emberson J, et al. Risk of intracerebral haemorrhage with alteplase after acute ischaemic stroke: a secondary analysis of an individual patient data meta-analysis. Lancet Neurol. 2016 Jun 8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#缺血性卒#
34
#Lancet#
31
#Neurol#
23
学习了,好文值得点赞!
42
#缺血性#
28