Crit Rev Oncol Hematol:结直肠癌错配修复状态的价值
2017-07-20 月下荷花 肿瘤资讯
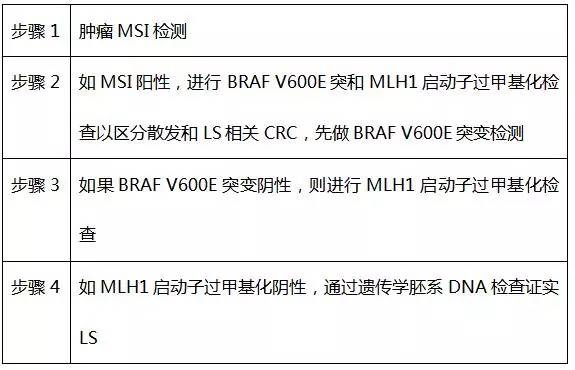
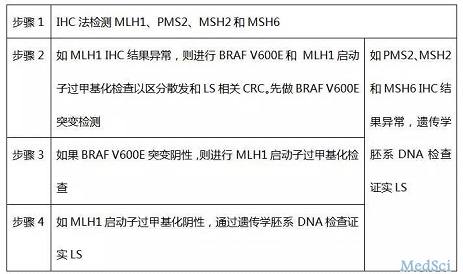
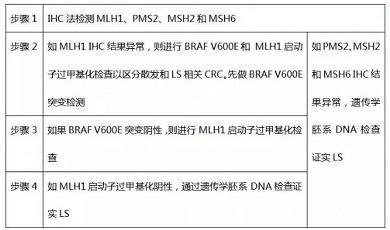
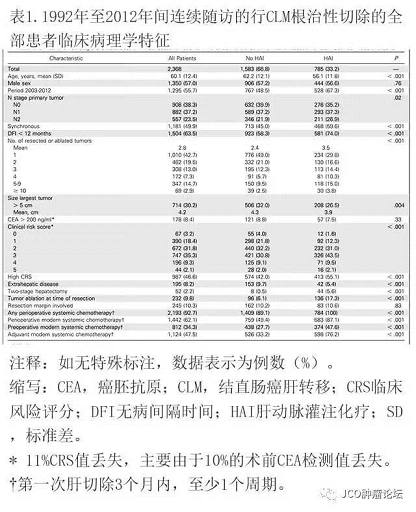
结直肠癌(CRC)是一组异质性疾病,传统上按分子途径分为二大类:染色体不稳定型(CIN)和微卫星不稳定型(MSI),CIN又分为3类共识分子亚型(CMS):CMS2、CMS3和CMS4,MSI或错配修复缺陷dMMR肿瘤多代表CMS1亚类,其诊断依靠PCR或IHC方法检测特定的微卫星序列是否扩增或MMR蛋白是否缺失。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
40
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
48
#EMA#
21
#结直肠#
27
学习了,谢谢
40
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了,点个赞吧!
46
签到学习了很多人
49