Eur Heart J:细菌培养阴性与培养阳性的感染性心内膜炎患者结局比较
2022-06-19 MedSci原创 MedSci原创
与细菌培养阳性的感染性心内膜炎相比,细菌培养阴性的感染性心内膜炎患者的长期死亡率更高。
全球范围内,感染性心内膜炎病死率高,其诊断仍然是一个挑战。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究的目的是比较细菌培养阳性的感染性心内膜炎与细菌培养阴性的感染性心内膜炎患者的临床特征和预后。
这是对ESC-EORP EURO-ENDO注册试验的辅助分析。该研究共纳入3113例在研究期间被诊断为感染性心内膜炎的患者。其中2590人(83.2%)为细菌培养阳性的感染性心内膜炎,而523人(16.8%)为细菌培养阴性的感染性心内膜炎。

1488例(48.1%)患者在住院期间接受了心脏手术治疗,1259例(48.8%)患者为细菌培养阳性的感染性心内膜炎和229例(44.5%)患者为细菌培养阴性的感染性心内膜炎。细菌培养阴性的感染性心内膜炎是1年死亡率的预测因子[风险比(HR)为1.28, 95%可信区间(CI)为1.04-1.56],而手术与生存率显著相关(HR为0.49, 95%CI为0.41-0.58)。
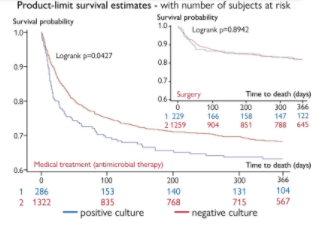
药物治疗组细菌培养阴性的感染性心内膜炎患者的1年死亡率明显高于细菌培养阳性的感染性心内膜炎患者,但手术组细菌培养阴性的感染性心内膜炎与细菌培养阳性的感染性心内膜炎患者的1年死亡率无显著差异。
由此可见,目前对EURO-ENDO注册试验的分析证实,与细菌培养阳性的感染性心内膜炎相比,细菌培养阴性的感染性心内膜炎患者的长期死亡率更高。这种差异只在单独接受药物治疗的患者中存在,而在接受手术的患者中则不然,手术与降低死亡率相关。还需要进一步的研究来提高感染性心内膜炎的病因诊断,并尽早识别细菌培养阴性的感染性心内膜炎病例。
原始出处:
William K.F. Kong,et al.Outcomes of culture-negative vs. culture-positive infective endocarditis: the ESC-EORP EURO-ENDO registry.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehac307/6604405?redirectedFrom=fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#感染性#
32
#内膜#
38
获益匪浅
29
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
26
#心内膜炎#
54
#ART#
25
#患者结局#
38
#细菌培养#
44
#HEART#
32