Stroke:去铁胺对基于血肿体积患者结局的影响
2021-11-21 MedSci原创 MedSci原创
在中度HV患者中,去铁胺治疗的患者比安慰剂治疗的患者达到改良的Rankin量表评分0-2的比例更大。对于小型或大型的HV,治疗效果不显著。这些结果具有重要的试验和治疗意义。
血肿体积是脑出血后预后的重要决定因素。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员评估了铁螯合剂去铁胺对出血患者功能结果的影响是否因血肿体积而异。

根据脑内出血去铁胺治疗试验(i-DEF)的事后分析;参与者根据基线血肿体积进行分类(小<10mL,中等10-30mL,大>30mL)。有利的结局定义为第180天时改良的Rankin量表评分为0-2;其次是在第90天时改良的Rankin量表评分。Logistic回归用于根据血肿体积评估的差异化治疗效果。
291名受试者被纳入治疗分析;121例患者为小型、114例患者为中型和56例患者为大型血肿体积。270/291名受试者(111名小型、105名中等和54名大型血肿体积)获得了第180天改良后的Rankin量表分数。
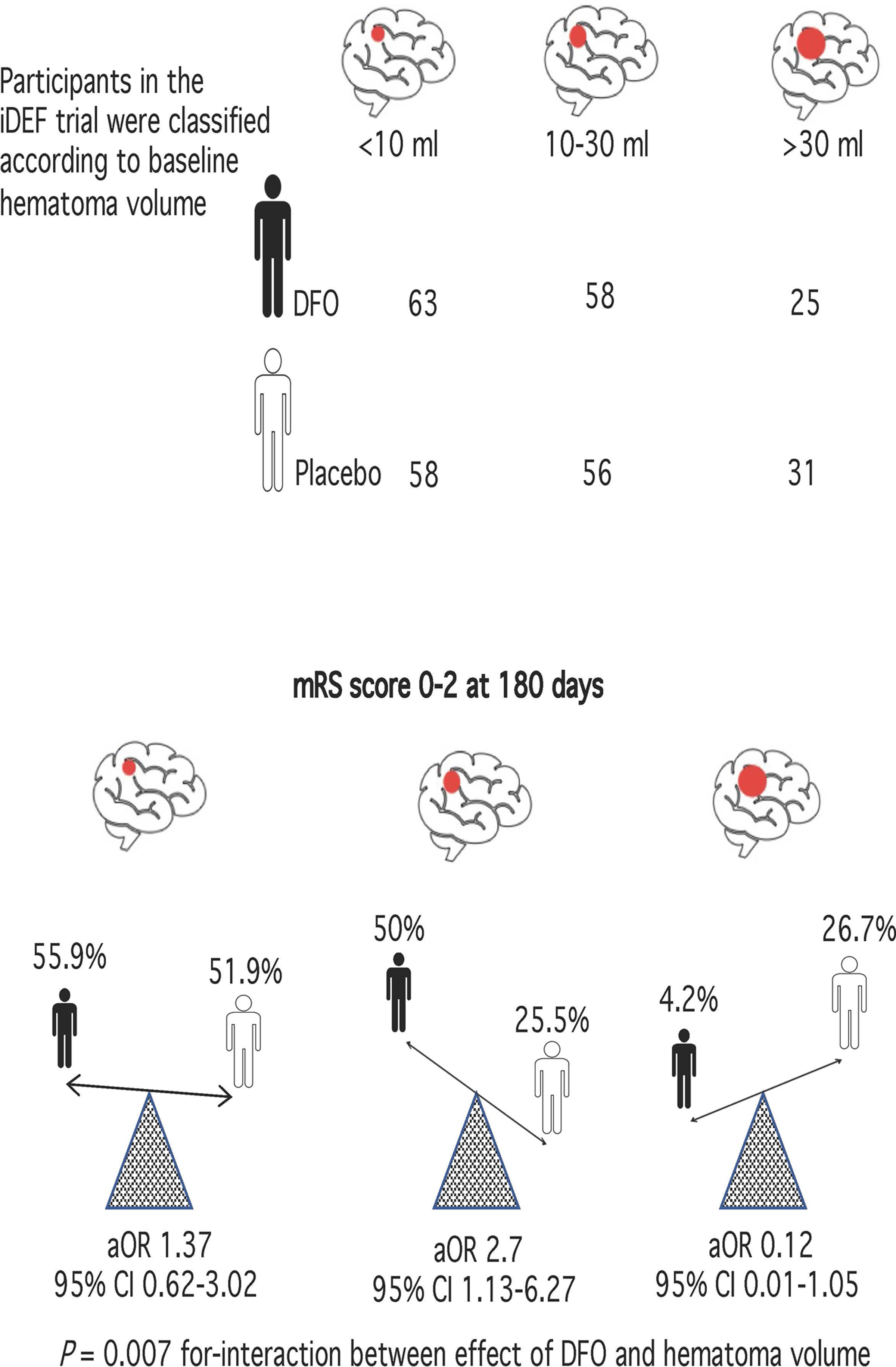
根据血肿体积的大小,治疗对第180天的结局有不同的影响(相互作用的P=0.0077);50%(27/54)的去铁胺治疗的中度血肿体积患者有良好的结局,而安慰剂治疗的受试者为25.5%(13/51)(调整后的比值比为2.7[95%CI为1.13-6.27];P=0.0258)。对于小(调整后的比值比为1.37[95%CI为0.62-3.02])或大(调整后的比值比为0.12[95%CI为0.01-1.05])血肿体积,治疗效果不显著。第90天的结局也相当(相互作用P=0.0617)。敏感性分析产生了类似的结果。
由此可见,在中度血肿体积患者中,去铁胺治疗的患者比安慰剂治疗的患者达到改良的Rankin量表评分0-2的比例更大。对于小型或大型的血肿体积,治疗效果不显著。这些结果具有重要的试验和治疗意义。
原始出处:
Chenchen Wei.et al.Effect of Deferoxamine on Outcome According to Baseline Hematoma Volume: A Post Hoc Analysis of the i-DEF Trial.stroke.2021.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.035421
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#血肿#
52
#患者结局#
30
学习了,谢谢分享
59
冲
44
冲
63