Neurology:前瞻性队列研究: 多多摄入类黄酮,或改善帕金森病患者死亡率!
2022-02-11 Naomi MedSci原创
近日,研究人员前瞻性地研究诊断前后类黄酮摄入量与PD患者死亡风险之间的关系。在PD患者中,黄酮类化合物的摄入量较高,尤其是花青素和黄酮 -3- 醇,以及富含黄酮类化合物的食物,或与PD死亡率更低有关。
帕金森病(PD)大幅降低患者生活质量,增加发病率和死亡率的风险。帕金森病患者的死亡风险高于一般人群,甚至可能高于其他常见慢性病患者,如大肠癌、卒中、冠心病及慢性阻塞性肺病。然而,少有研究探讨可改变的风险因素如饮食因素对PD患者生存的潜在作用。多种饮食成分中,例如类黄酮和富含类黄酮的食物,以前曾被证明与发生PD的风险较低有关。
类黄酮是植物衍生的多酚类分子,天然存在于多种水果、蔬菜和一些饮料(例如茶和红酒)中。摄入后,它们会迅速代谢,这些代谢物可以通过血脑屏障产生多种功能,例如减轻氧化应激、炎症和动脉粥样硬化。有证据表明,它们可以减少脑内一氧化氮合酶和黄嘌呤氧化酶活性造成的损伤,因此它们的神经保护潜能很有价值。尽管最近就帕金森病进行了多项动物实验,以检验类黄酮化合物的潜在治疗作用,但缺乏人体研究中黄酮类化合物与PD预后之间关系的证据。
患有PD的人一般会出现吞咽困难、颚部僵硬、刀叉和食物处理能力下降(即吞咽困难)、可能导致进食富含黄酮类化合物的食物(例如水果/蔬菜)和疾病预后不良。为了最小化PD运动症状发作后由于吞咽困难和其他相关运动障碍引起的逆向因果关系的可能性,并为自 PD临床前阶段以来,饮食在PD疾病进程中的作用提供证据,研究人员使用PD诊断前后收集的黄酮类摄入量作为这项研究的主要暴露量。
虽然黄酮类化合物有潜在的神经保护作用,但是仍然缺乏证据证明它们在提高帕金森氏症患者的存活率方面的作用。近日,有研究人员前瞻性地研究诊断前后类黄酮摄入量与PD患者死亡风险之间的关系。
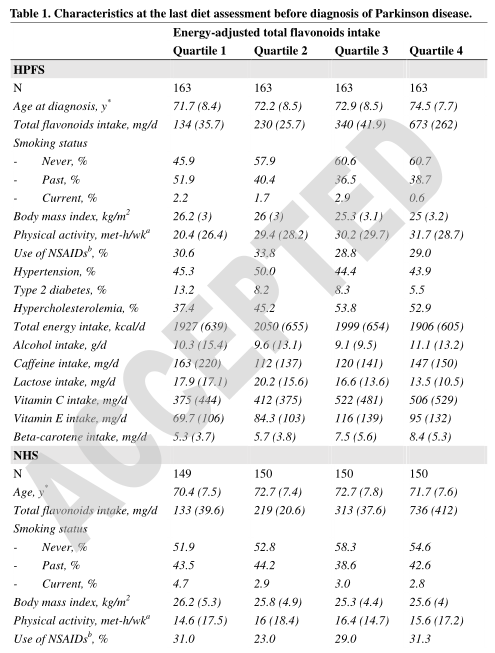
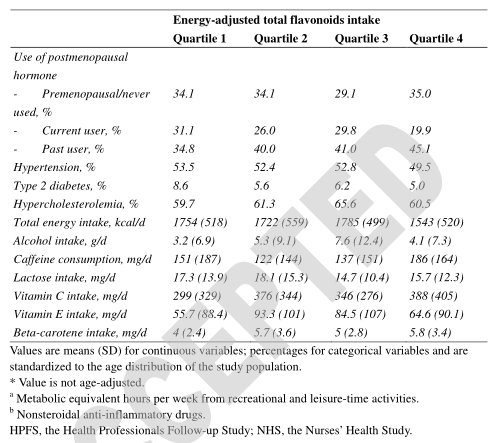
研究共纳入599名来自the Nurses’ Health Study的599名女子和652名来自the Health Professionals Follow-up Study的女子。饮食中总黄酮及其亚类的摄入量以及主要富含黄酮类的食物(茶、苹果、浆果、橙汁和橙汁以及红酒),每4年根据一份有效的食物频率问卷重复进行评估。死亡率是通过国家死亡指数和国家生命统计记录确定的。
- 共记录了32-34年间944例死亡病例;
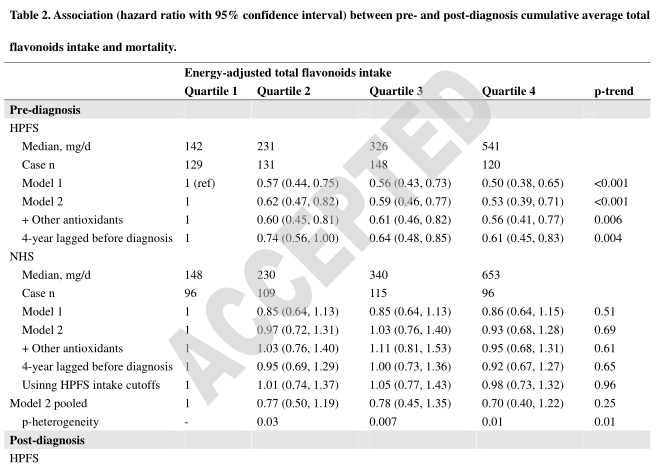
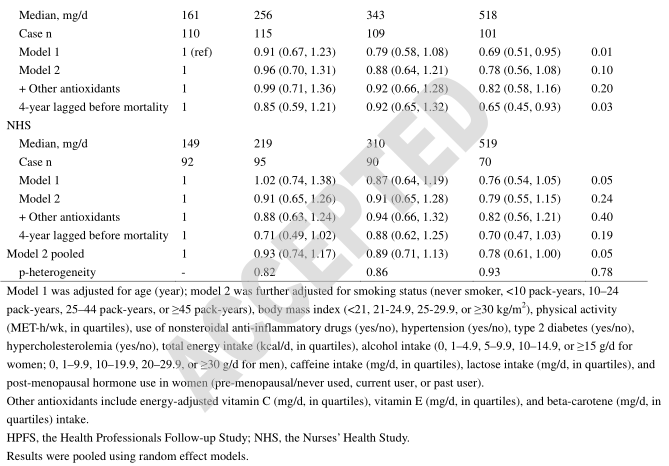
- 与两个极端的四分位数相比,男性在确诊前摄入较高的总黄酮量与未来全因死亡风险较低有关(危险比[ hr ] = 0.53,95% ci: 0.39,0.71; p-trend < 0.001) ,而女性则不然(hr = 0.93,95% ci: 0.68,1.28; p-trend = 0.69)。
- 极端四分位数比较的汇总心率为0.70(95% ci: 0.40,1.22; p-趋势 = 0.25) ,异质性显著(p = 0.01);
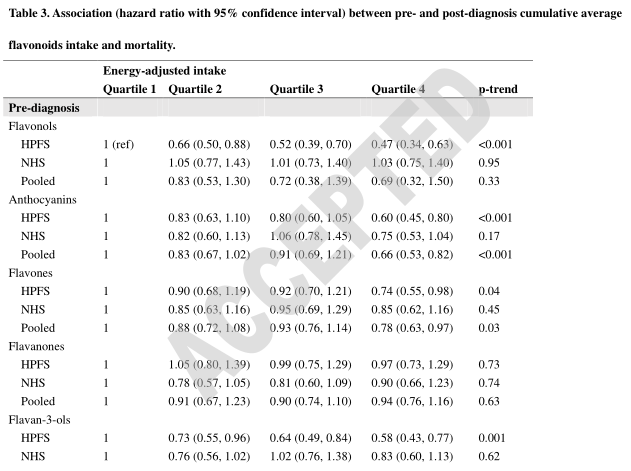
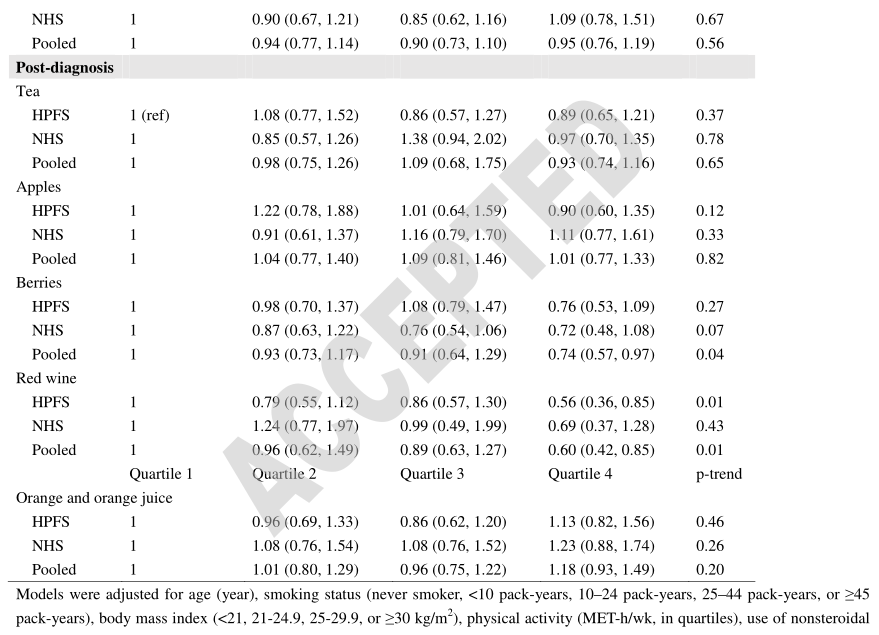
- 对于类黄酮亚类,诊断前最高四分之一的花青素、黄酮和黄酮 -3- 醇摄入量与最低四分之一的人相比,死亡风险较低(合计 hr = 0.66、0.78和0.69,所有人均 p < 0.05) ; 对于浆果和红酒,每周摄入≥ 3的参与者死亡风险较低(pooled hr = 0.77,(95% ci: 0.58,1.02)和0.68(95% ci: 0.51,0.91);
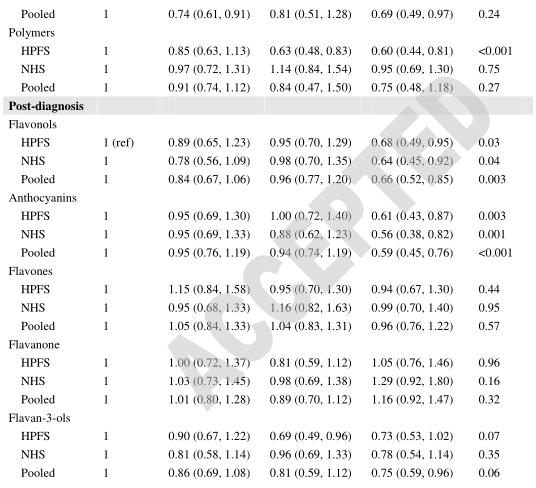
- 在PD诊断后,总黄酮类化合物,包括黄酮醇、花青素、黄酮 -3- 醇和聚合物,浆果和红酒的消耗量较大,与较低的死亡风险相关(p < 0.05);
在帕金森病患者中,黄酮类化合物的摄入量较高,尤其是花青素和黄酮 -3- 醇,以及富含黄酮类化合物的食物,如浆果和红酒,可能与此死亡率更低有关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#前瞻性队列#
48
#黄酮#
33
#Neurol#
35
#帕金森病患者#
41
#前瞻性#
35
#患者死亡#
38
学到了#学习#
51
学习了
38
#前瞻性队列研究#
32
坚持学习
47