JCEM:原发性甲状旁腺功能亢进患者甲状旁腺切除术与非手术治疗的肾结石事件
2022-04-04 MedSci原创 MedSci原创
而非手术治疗的患者相比,原发性甲状旁腺功能亢患者甲状旁腺切除术仍是肾结石的风险事件,尽管肾结石事件的调整风险随着时间的推移有所下降。
原发性甲状旁腺功能亢进与肾结石风险增加有关。当比较甲状旁腺切除术和非手术治疗后的结石事件时,很少有研究考虑到原发性甲状旁腺功能亢进的严重程度或结石风险。
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在比较甲状旁腺切除术和非手术治疗的原发性甲状旁腺功能亢进患者肾结石事件的发生率。
该纵向队列研究采用退伍军人健康管理局综合医疗保健系统进行了倾向评分逆概率加权和多变量Cox比例风险回归分析。该研究纳入了44978例诊断为原发性甲状旁腺功能亢进的患者(2000-2018),患者随访了2年。5244例(11.7%)患者接受甲状旁腺切除术。该研究的主要结局指标为临床显著的肾结石事件。
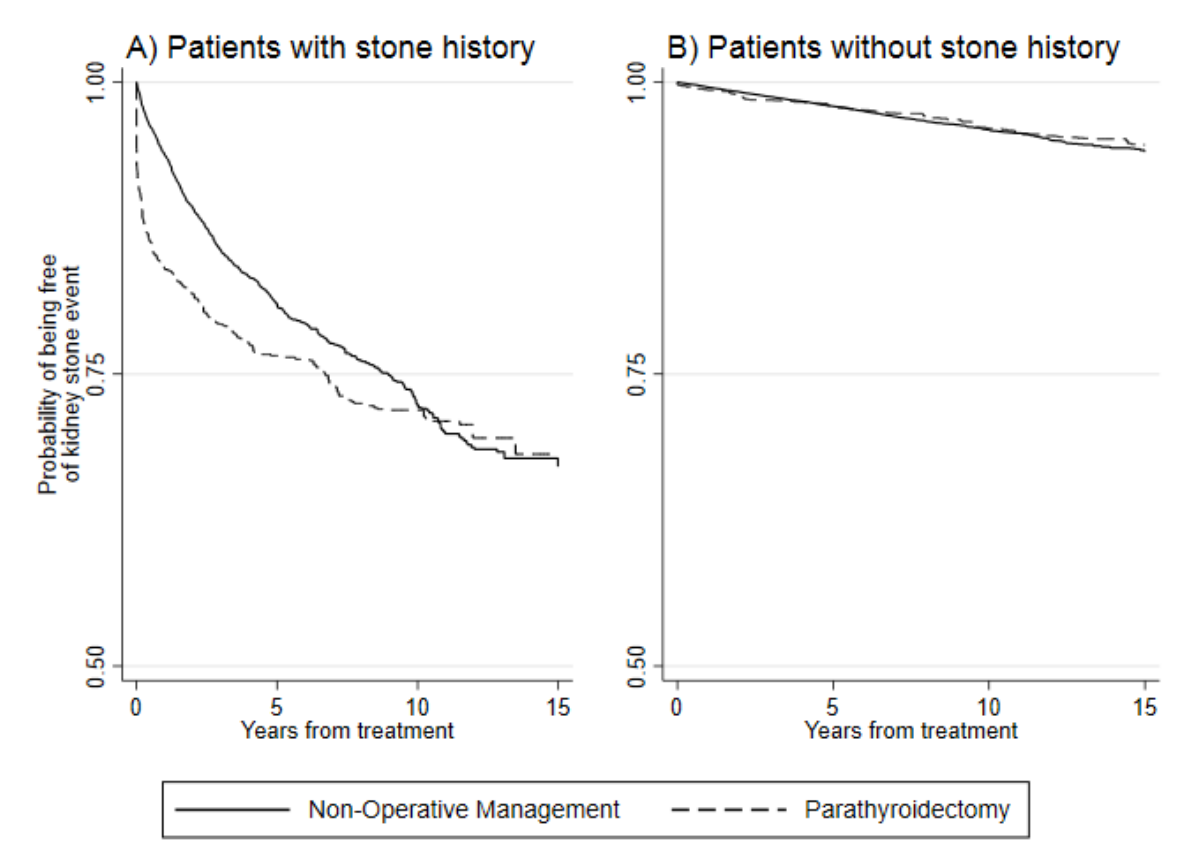
该队列参与者的平均年龄为66.0岁,男性占87.8%,白人占66.4%。接受甲状旁腺切除术的患者有较高的平均血清钙水平(11.2 vs. 10.8mg/dL),更有可能有肾结石事件的病史。在有基线肾结石病史的患者中,甲状旁腺切除术患者(平均随访5.6年)患肾结石事件的未调整发生率为30.5%,而非手术治疗的患者(平均随访5.0年)为18.0%。接受甲状旁腺切除术的患者复发肾结石事件的调整后风险更高(风险比[HR]为1.98, 95%CI为1.56-2.51);然而,这种相关性随着时间的推移而下降(甲状旁腺切除术*时间HR为0.80, 95%CI为0.73-0.87)。
由此可见,而非手术治疗的患者相比,原发性甲状旁腺功能亢患者甲状旁腺切除术仍是肾结石的风险事件,尽管肾结石事件的调整风险随着时间的推移有所下降。
原始出处:
Carolyn D Seib,et al.Kidney stone events following parathyroidectomy vs. non-operative management for primary hyperparathyroidism.JCEM.2022.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgac193/6562390
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#JCEM#
31
#JCE#
38
#原发性#
56
#切除术#
38
10余年,临床上就遇到2例甲旁亢病人?
38
#手术治疗#
54
#甲状旁腺功能亢进#
46
#非手术治疗#
44
#甲状旁腺#
42
#甲状旁腺切除术#
37