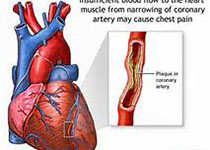
JACC:SGLT1基因突变引起的葡萄糖吸收减少可降低心血管代谢风险
2018-10-05 MedSci MedSci原创
SGLT1基因的功能缺失性突变会导致一种罕见的葡萄糖吸收障碍综合征,如果不治疗的话会于婴儿期死亡。本研究的目的旨在寻找SGLT1基因的功能性变异,并评估其对临床的影响。本研究对ARIC临床研究中的参与者进行了全外显子测序,并对SGLT1基因的功能性错义变异与2小时口服糖耐量试验结果的相关性进行评估。最终共纳入5687例研究对象(平均年龄54 ± 6岁,男性占47%)。分析结果显示,携带三种错义突变
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SGLT#
28
#SGLT1#
30
#心血管代谢#
37
#JACC#
28
#ACC#
25
学习了
72