Circ-Heart Fail:急性心肌梗死和心力衰竭相关心源性休克的临床特征、住院病程和1年结局比较
2022-05-13 MedSci原创 MedSci原创
HF-CS患者较年轻,尽管心功率输出较低,肺毛细血管楔形压较高,但接受血管加压药或临时机械循环支持的可能性较小。
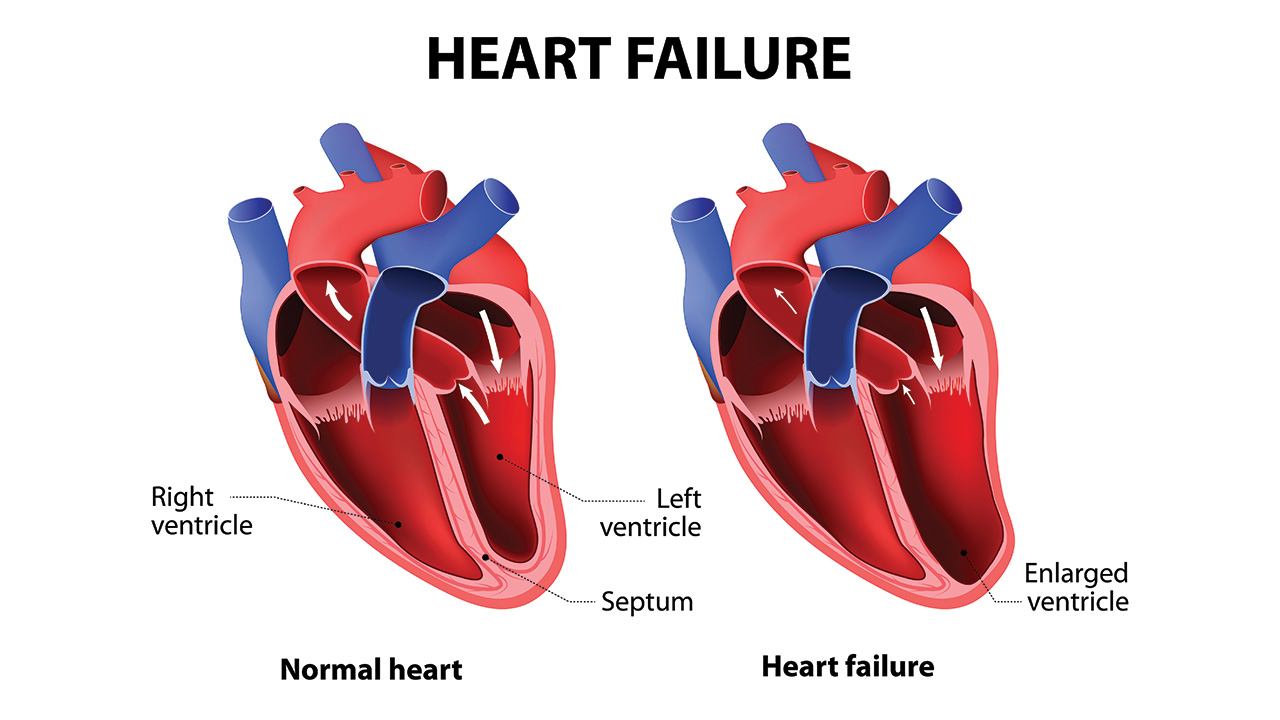
心源性休克(CS)是一种血流动力学复杂综合征,其病因较多,发病率和死亡率也很高。与急性心肌梗死与(AMI)相关的CS(AMI-CS)相比,人们对与心力衰竭相关的心源性休克(HF-CS)患者的临床特征、住院过程和纵向结局知之甚少。
近日,心血管领域权威杂志Circulation: Heart Failure上发表了一篇研究文章,研究人员在一个单中心登记处评估了520例(219例AMI-CS患者,301例HF-CS患者)连续就诊的CS患者(2017年1月3日,2019年12月31日)的住院和1年结局。

受试者平均年龄为61.5±13.5岁,71%为男性,22%为黑人,63%伴有慢性肾脏疾病。相比于AMI-CS患者,HF-CS患者更年轻(58.5 vs. 65.6岁,P<0.001),更少发生心脏骤停(15.9% vs. 35.2%,P<0.001),更少使用血管加压素(61.8% vs. 82.2%,P<0.001),更高的肺动脉搏动指数(2.14 vs. 1.51,P<0.01),更低的心功率输出(0.64 vs. 0.77W,P<0.001)。P<0.01),更高的肺毛细血管楔形压(25.4 vs. 22.2mmHg,P<0.001)。HF-CS患者接受的短期机械循环支持更少(34.9% vs. 76.3%P<0.001),大出血发生率更低(17.3% vs. 26.0%,P=0.02),住院死亡率也更低(23.9% vs. 39.3%,P<0.001)。
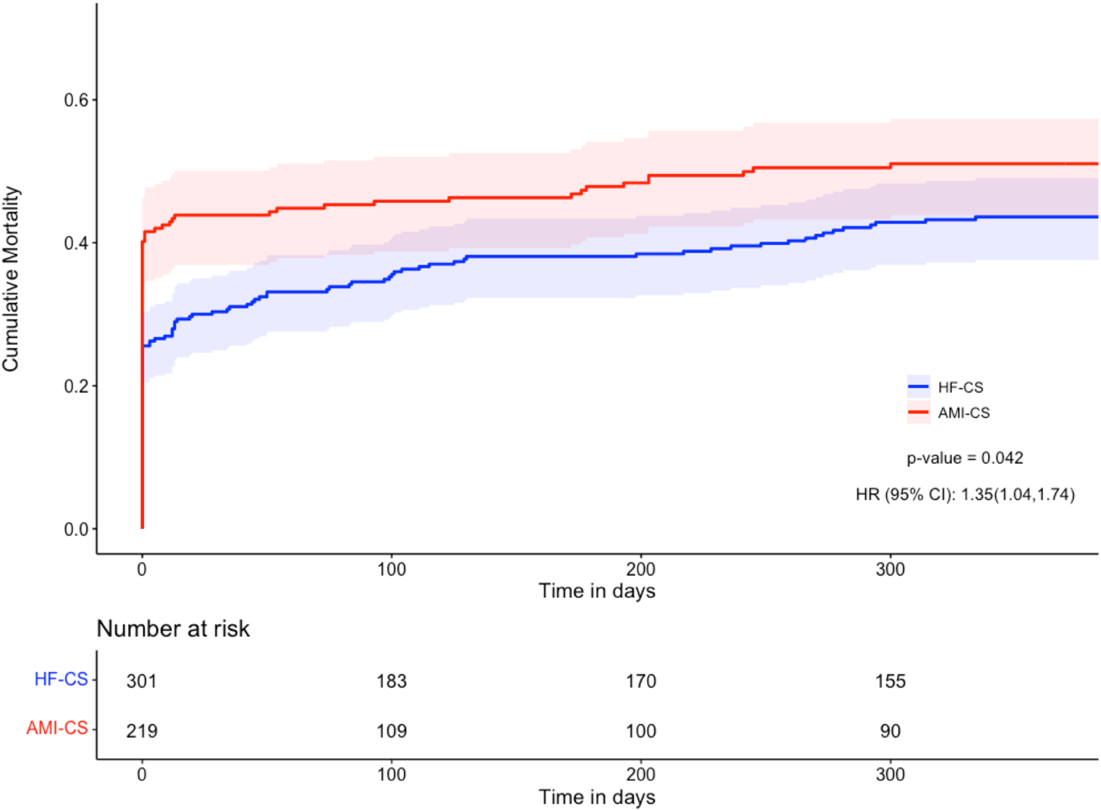
出院后,133例AMI-CS患者和229例HF-CS患者30天再入院率(19.5% vs. 24.5%,P=0.30)和主要不良心脑血管病事件(23.3% vs. 28.8%,P=0.45)相似。HF-CS患者的1年死亡率(n=123,42.6%)低于AMI-CS患者(n=110,52.9%,P=0.03)。HF-CS患者的1年累计死亡率也较低(log-rank检验,P=0.04)。
由此可见,HF-CS患者较年轻,尽管心功率输出较低,肺毛细血管楔形压较高,但接受血管加压药或临时机械循环支持治疗的可能性较小。尽管HF-CS患者的住院死亡率和1年死亡率较低,但两组患者出院后发生重大心血管和脑血管不良事件和30天再次入院的比例相似,这表明两组患者都需要仔细的长期随访。
原始出处:
Shashank S. Sinha, et al.Cardiogenic Shock From Heart Failure Versus Acute Myocardial Infarction: Clinical Characteristics, Hospital Course, and 1-Year Outcomes. Circulation: Heart Failure. 2022;https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.121.009279
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床特征#
54
好
57
#心源性休克#
0
#ART#
48
#HEART#
57
#心源性#
44
很好
65
不错,学习了。
64