JAMA Pediatrics:剖宫产会增加儿童肥胖风险
2016-09-07 MedSci MedSci原创
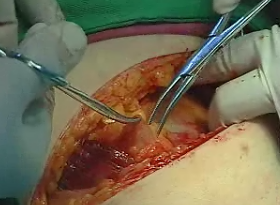
剖宫产是美国最常见的外科手术,约有1/3的产妇经由剖宫产分娩。剖宫产分娩的新生儿最常出现的健康问题是呼吸系统疾病,同时有研究指出,经剖宫产分娩的新生儿成年后呼吸系统健康问题依旧不可忽视。 哈佛大学公共卫生学院的研究人员对GUTS研究参与者进行评估,旨在探究剖宫产与儿童和年轻人肥胖之间的关联。研究对象包括15271名女性分娩的22068名儿童,其中共有4921名儿童(22.3%)通过剖宫产出生。研究
剖宫产是美国最常见的外科手术,约有1/3的产妇经由剖宫产分娩。剖宫产分娩的新生儿最常出现的健康问题是呼吸系统疾病,同时有研究指出,经剖宫产分娩的新生儿成年后呼吸系统健康问题依旧不可忽视。
哈佛大学公共卫生学院的研究人员对GUTS研究参与者进行评估,旨在探究剖宫产与儿童和年轻人肥胖之间的关联。研究对象包括15271名女性分娩的22068名儿童,其中共有4921名儿童(22.3%)通过剖宫产出生。研究结果表明,女性接受剖宫产后较孕前BMI更高,且更易在下次妊娠时患妊娠糖尿病与子痫前期。经剖宫产分娩的儿童较阴道分娩的儿童肥胖的风险增加15%。此外,相比经阴道分娩的兄弟姐妹,经剖宫产分娩的儿童肥胖的风险要高出64%。研究结果发表在JAMA Pediatrics。
其他研究表明,分娩方式对新生儿肠道微生物群有明显影响。经剖宫产分娩的新生儿肠道葡萄球菌更多,而双歧杆菌数量更少,这与超重和肥胖的风险增加有关。且研究人员指出,他们发现经剖宫产分娩可明显增加儿童和成年人早期肥胖的风险。但是他们表示仍需进行更进一步的研究,以获取孕妇在孕早、中、晚期的相关数据,使研究结果更具有准确性。
[1] Cesarean delivery may increase risk of childhood obesity.MNT.7.Sept.2016
[2] Changzheng Yuan, Sc.D.et al.,Association between cesarean birth and risk of obesity in offspring in childhood adolescence, and early adulthood. JAMA Pediatrics.6 Sept.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Pediatric#
29
#DIA#
34
#PE#
41
谢谢分享!
74
谢谢分享!
79
学习了谢谢
70
学习了。。
67
继续学习。。。
69
不错的内容。
23
学习学习。。。
37