J Clin Oncol:醋酸阿比特龙在去势抵抗、雄激素受体表达的唾液腺癌(SGC)患者中的疗效
2021-10-02 yd2015 MedSci原创
研究表明,阿比特龙联合促黄体生成素释放激素激动剂是去势抵抗、雄激素受体表达的唾液腺癌(SGC)患者有效并且安全的二线治疗。
涎腺导管癌(SDC)跟高级别乳腺导管癌具有相似的形态学和分子特征,表现为雄性激素受体(AR)表达;TP53突变 [55%], HRAS突变 [23%], 和 PIK3CA突变 [23%]; 以及ERBB2扩增 [35%]。AR表达存在90%以上的SDC患者和20%-30%的非其他特异(NOS)腺癌患者。雄激素受体阳性(AR)唾液腺癌(SGC)患者可从雄激素剥夺治疗(ADT)中获益。ADT失败后的最佳治疗方法尚不清楚。在这种情况下,治疗选择包括靶向特定的分子途径(如,人表皮生长因子受体2),或细胞毒性化疗。目前,二线的激素治疗还没有成功的研究。因此,国外团队开展了一项II期研究,评估醋酸阿比特龙在去势抵抗、雄激素受体表达的唾液腺癌(SGC)患者中的疗效。相关成果发表在Journal of Clinical Oncology杂志上。

该研究为单中心的II期研究,主要终点为客观有效率(ORR)。次要终点为疾病控制率(DCR)、安全性、无进展生存期(PFS)和总生存期(OS)。所有患者接受阿比特龙+强的松+促黄体生成素释放激素激动剂,直到进展或不可接受的毒性。
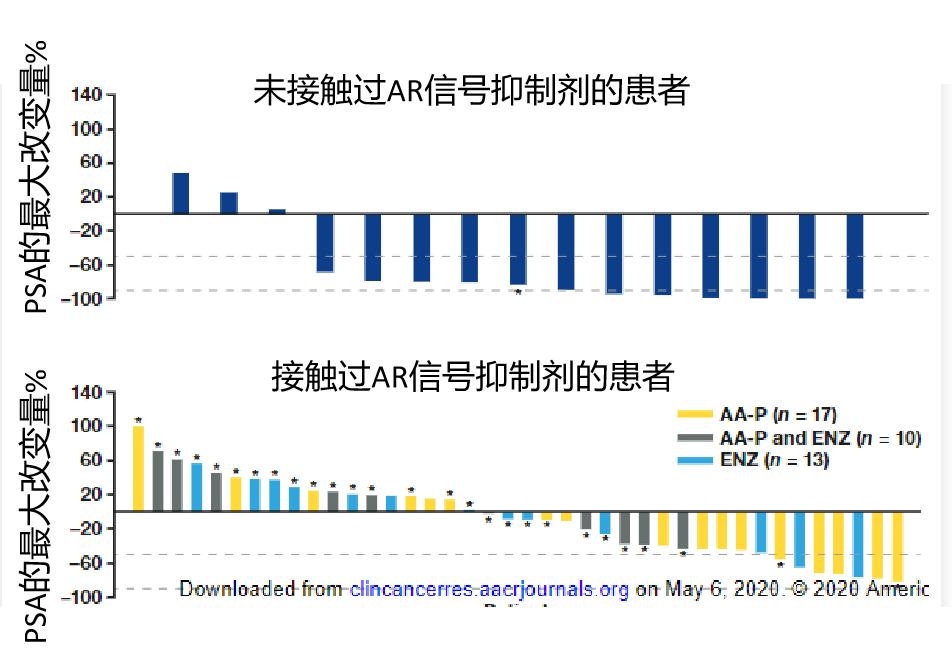
从2015年3月到2019年11月,24名患者(23名男性)纳入该研究。中位随访时间为9.47个月(95% CI, 5.66 - 20.56)。中位年龄为65.8岁(范围44-77),所有患者的ECOG评分为为0-1。19例(79%)为SDC, 5例(79%)为腺癌NOS。所有病例中AR均过表达。4例(3例SDC和1例腺癌NOS)中HER2扩增。
ORR为21%,中位DoR为5.82个月(95% CI, 4.24 - 10.76)。DCR为62.5%, 9例患者PD (37.5%)。三例患者仍在治疗。其余21例患者均因进展停用阿比特龙。中位治疗时间为3.93个月(范围为1.15-18.88)。
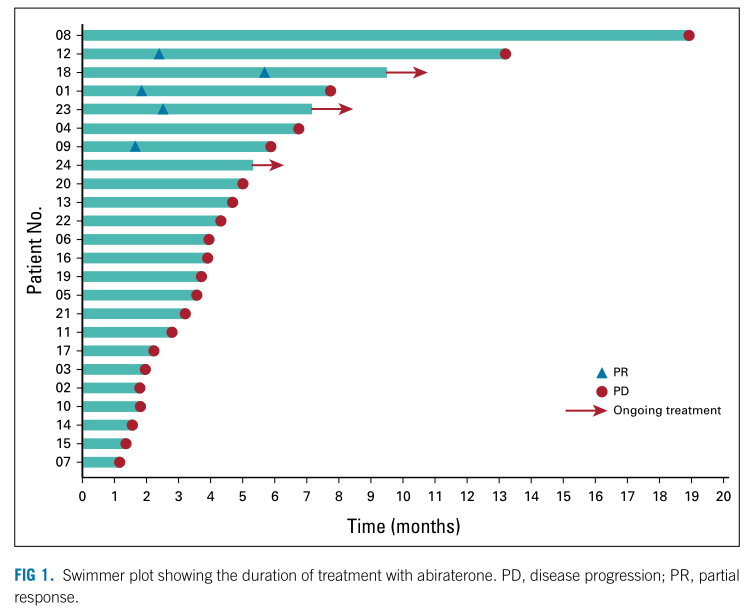
疗效
中位无进展生存期为3.65个月(95%CI, 1.94 - 5.89),中位OS为22.47个月(95%CI,6.74 –未达到)。12个月OS为66.59%(19例SDC患者为74.48%,5例腺癌NOS患者为50%,P=0.334)。从诊断为原发性SGC的中位OS为94.31个月(95% CI, 46.61 - NR)。

PFS和OS
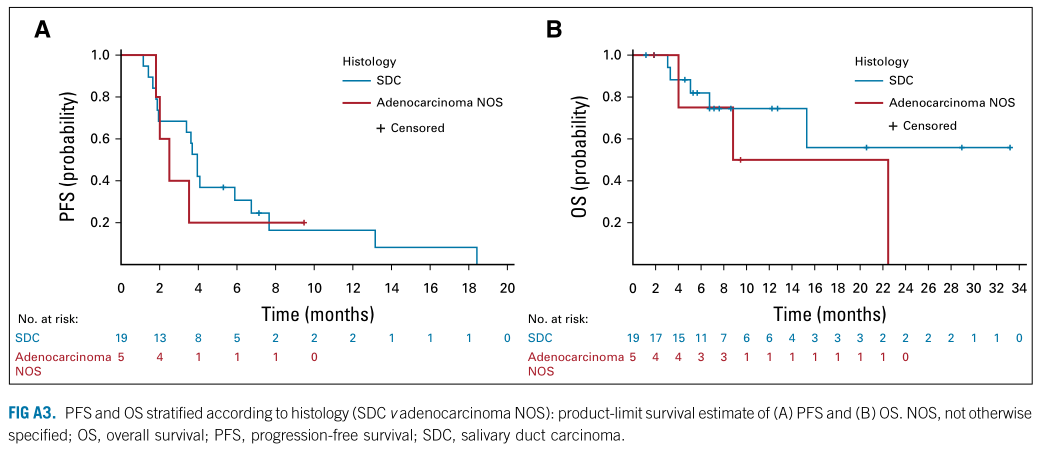
不同类型肿瘤的PFS和OS
92%的患者报告至少有1种不良反应(22例)。最常见的与药物相关的AEs为疲劳(38%)、潮红(29%)和低钾血症(17%)。6例(25%)患者出现3级AEs: 4例药物相关(2例疲劳,1例潮红,1例室上性心动过速),2例非药物相关(1例癌症相关疼痛,1例口干)。未观察到药物相关的4级和5级AEs。所以患者不需要减少剂量,也没有患者因为毒性停止治疗。
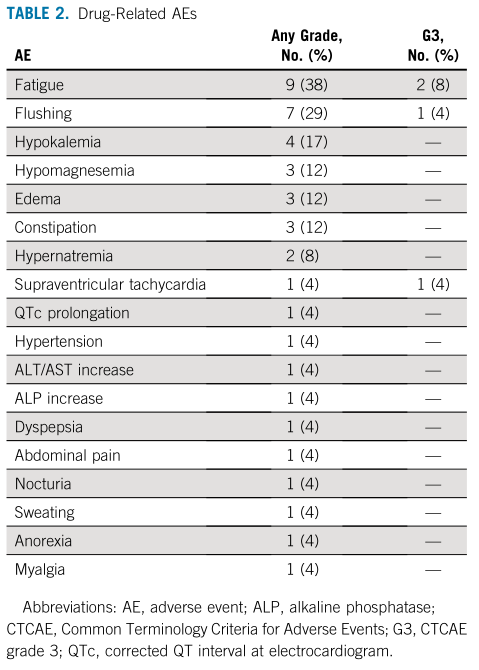
不良事件
综上,研究表明,阿比特龙联合促黄体生成素释放激素激动剂是去势抵抗、雄激素受体表达的唾液腺癌(SGC)患者有效并且安全的二线治疗。
原始出处:
Locati LD, Cavalieri S, Bergamini C, Resteghini C, Colombo E, Calareso G, Mariani L, Quattrone P, Alfieri S, Bossi P, Platini F, Capone I, Licitra L. Abiraterone Acetate in Patients With Castration-Resistant, Androgen Receptor-Expressing Salivary Gland Cancer: A Phase II Trial. J Clin Oncol. 2021 Oct 1:JCO2100468. doi: 10.1200/JCO.21.00468. Epub ahead of print. PMID: 34597119.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#唾液腺#
27
#Oncol#
26
#雄激素受体#
35
#醋酸阿比特龙#
33