Nat Commun:肿瘤抑制蛋白反而促进癌症生长
2017-01-28 MedSci MedSci原创
来自杜兰大学的研究人员发现一种此前被认为是肿瘤抑制因子的蛋白PHLDB3事实上可以促进胰腺癌、前列腺癌、直肠癌、乳腺癌、肺癌及一些其他常见癌细胞的生长。这项新发现可能揭示了肿瘤克服关键肿瘤抑制因子p53的机制,这项新发现最近发表在《Nature Communications》上,将有助于开发出靶向一系列肿瘤的诊断和治疗方法。“现在我们已经发现了这种分子的促癌作用,因此我们可以把它作为抗癌靶标。”来
来自杜兰大学的研究人员发现一种此前被认为是肿瘤抑制因子的蛋白PHLDB3事实上可以促进胰腺癌、前列腺癌、直肠癌、乳腺癌、肺癌及一些其他常见癌细胞的生长。这项新发现可能揭示了肿瘤克服关键肿瘤抑制因子p53的机制,这项新发现最近发表在《Nature Communications》上,将有助于开发出靶向一系列肿瘤的诊断和治疗方法。
“现在我们已经发现了这种分子的促癌作用,因此我们可以把它作为抗癌靶标。”来自图兰(Tulane)大学的研究领导者Hua Lu博士说道,“这个靶标很有希望用于开发抗肿瘤药物,将这些药物与化疗联合将更有效、更安全。”
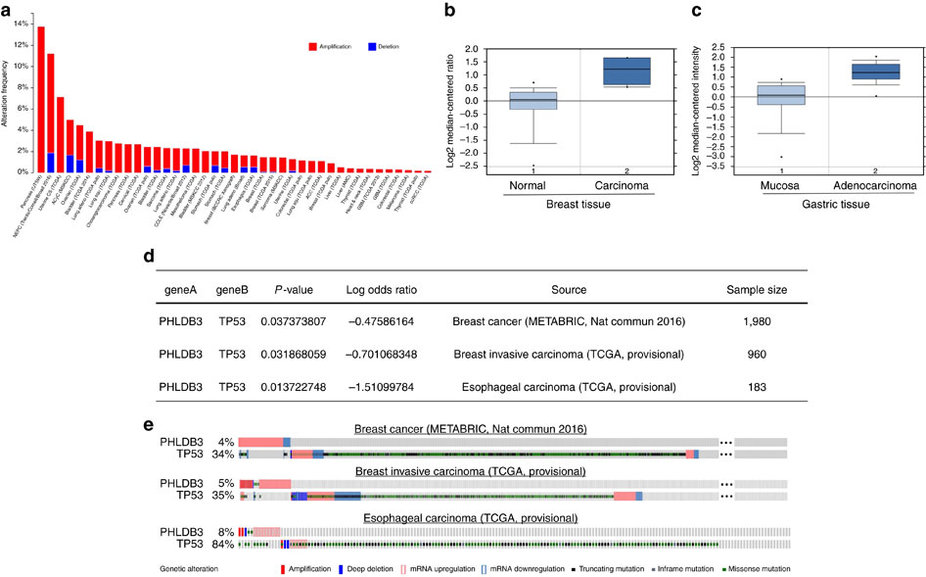
Figure 3: High expression of PHLDB3 is found in multiple cancers and mutually exclusive to TP53 mutations in some cancers.(a) TCGA database was searched, and the data were modified from the cBioPortal for Cancer Genomics (http://www.cbioportal.org/). (b,c) The expression profile of PHLDB3 in cancers and normal tissues was searched in Oncomine Gene Browser (http://www.oncomine.org/). The results in TCGA Breast Dataset (b) and DErrico Gastric Dataset (c) are shown. (d) Analysis of mutual exclusivity was retrieved from cBioPortal and gene alteration status of PHLDB3 and TP53 of individual sample is depicted in e.
研究人员早就知道p53可以使细胞在恶化前发生DNA损伤而死亡,以此防止肿瘤形成。P53蛋白的表达由两种基因控制(MDM2和MDMX),这两个基因可以调节P53的表达量,这两个基因及p53的过表达都有害,因此p53和这两个基因之间的表达平衡保持了细胞的正常发展。Lu和他的团队发现PHLDB3可以和MDM2一起抑制p53的表达,从而促进肿瘤生长。这个蛋白还可能导致了一些晚期肿瘤对治疗产生抗性。
为了确定PHLDB3是一个较好的药物靶点,Lu说他的团队下一步的工作将是通过动物模型进一步确定PHLDB3的促癌作用是否依赖于p53。他认为明白这个蛋白在细胞信号通路及机体正常发育过程中的生物学机制是非常重要的,同时也很有必要确定这个蛋白在人类肿瘤发生、发展和产生耐药性过程中的具体作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
32
#肿瘤抑制#
36
#肿瘤抑制蛋白#
32
#Nat#
24
很有意义的文章,希望临床早日应用
59
最新研究进展
61
基因太神奇了
65
新能点看看
56