ASCO 2020:MEK162(贝美替尼)联合伊马替尼治疗晚期胃肠道间质瘤II期临床研究
2020-05-23 医学论坛网 医学论坛网
背景:ETV1和KIT是胃肠道间质瘤家族特异的主转录因子和信号生存因子。在临床前模型中,贝美替尼(BINI)抑制ETV1以及伊马替尼抑制KIT在抑制胃肠道间质瘤肿瘤发生和发展中具有协同作用。这项单臂I
背景:ETV1和KIT是胃肠道间质瘤家族特异的主转录因子和信号生存因子。在临床前模型中,贝美替尼(BINI)抑制ETV1以及伊马替尼抑制KIT在抑制胃肠道间质瘤肿瘤发生和发展中具有协同作用。这项单臂II期研究旨在测试贝美替尼+伊马替尼作为一线治疗晚期胃肠道间质瘤患者的疗效。
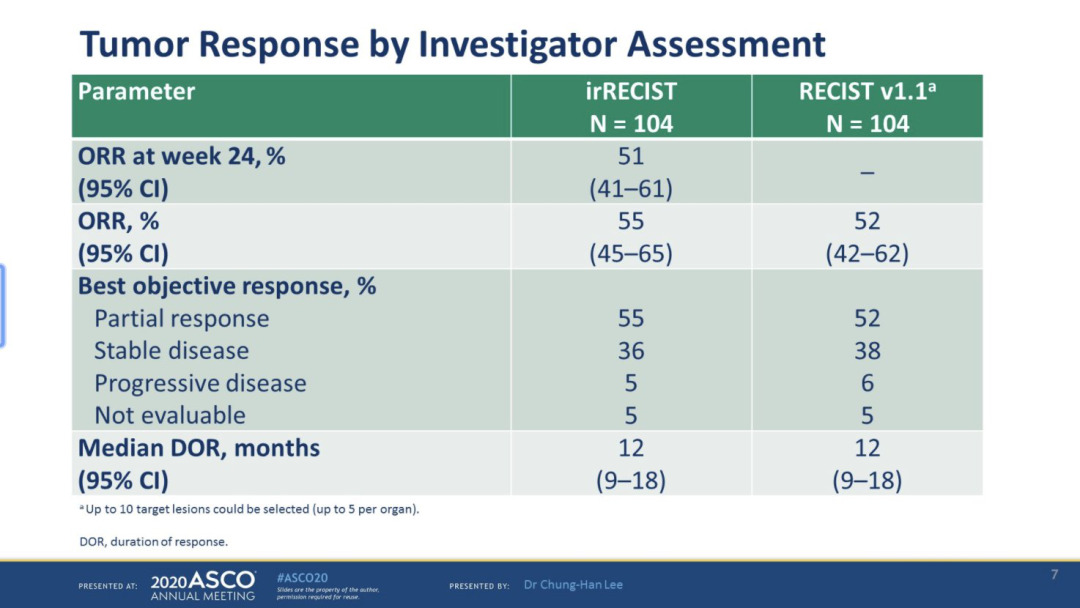
方法:未经治疗的晚期胃肠道间质瘤成人患者接受伊马替尼(每天400mg)加贝美替尼(每天两次30mg),为期28天。主要终点(EP)为RECIST1.1标准下的客观缓解率(ORR)(完全缓解[CR] +部分缓解[PR])该研究旨在检测仅伊马替尼的ORR改善20%(不可接受的比率为45%;可接受的比率为65%)。使用精确的二项式检验,单侧I型误差为0.08,II型误差为0.1,需要44名患者的样本量。超过24例患者达到PR,可判定有效。次要终点按Choi和EORTC标准得出的RR,可切除性转化率(RCR),无进展生存期(PFS),总生存期(OS)和长期不良事件。对MSK-IMPACT法检测的表观肿瘤基因组学、MSK-ACCESS法检测的cfDNA、ETV1蛋白水平和转录组以及信号传导抑制进行相关性检验。
结果:在2020年1月31日数据截止时,39例胃肠道间质瘤患者中,有38例可进行主要终点评估,其中包括3例KIT/PDGFRA野生型患者。中位年龄为60岁(范围为29-78),女性占比为29%。
38例患者中26例确认达到PR;最佳ORR为68.4%(双侧95%CI,51%-83%;单侧90%CI,57%-100%)。9例患者中8例治疗后达到可切除;,RCR为88.9%(95%CI,52-100%)。目前仍有13例患者在试验观察(2~159周)。9例患者因疾病进展而中止试验(11-159周),1例患者在3个月内进展,表现为原发耐药。3/4级毒性包括CPK升高(无症状,61%),中性粒细胞减少(11%),斑丘疹(8%),贫血(8%)。没有观察到意外的毒性。后续报道将介绍MSK-IMPACT、MSK通路和成对肿瘤活检的相关性。
结论:该研究达到了其主要终点。 贝美替尼加伊马替尼在未治疗的晚期胃肠道间质瘤中非常有效,长期治疗相关毒性可判可控。在胃肠道间质瘤的一线治疗中,与伊马替尼直接比较,该联合策略值得进一步评价。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#I期临床#
24
#晚期胃肠道间质瘤#
54
#II期临床研究#
17
#ASC#
26
#MEK#
24
#贝美替尼#
22
#ASCO 2020#
23
#胃肠道#
33
#间质瘤#
26
#II期临床#
22