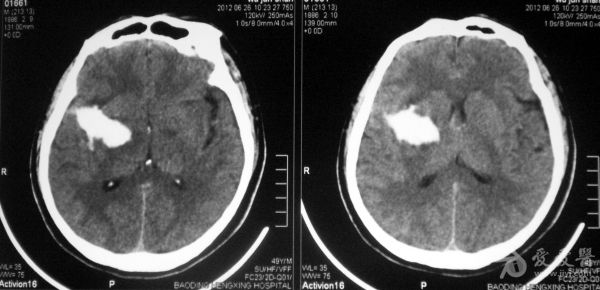
Stroke:脑出血患者是否应该服用他汀类药物?
2015-06-16 大鹏 cmt
有关ICH患者使用他汀类药物一直存在争议。近期,美国心脏学会和美国卒中学会(AHA/ASA)于《卒中》(Stroke)杂志发布了新版脑出血(ICH)管理指南,或许该指南相关内容能初步解答上述问题。在预防ICH复发方面,指南推荐,尚缺乏足够证据限制ICH患者服用他汀类药物(Ⅱb,C)。以下为该指南制定此项指导意见的相关证据。 SPARC
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#他汀类药#
31
ICH患者应该还是要服用他汀类药物
132
需要好好研究
114
看看
126
观
114
需要看看原文和入选的试验
106
复杂
73