Cell:CDK7可能成为三阴性乳腺癌划时代性靶点
2015-09-25 MedSci MedSci原创
背景介绍 CDK7是个跟细胞周期有关的蛋白激酶, THZ1是CDK7共价抑制剂。其实这个分子还有控制转录起始和延伸的作用。作者之前的团队报道过靶向CDK7的肿瘤治疗效应。 这篇文章是一个延续性研究,在三阴性乳腺癌,发现了那么一簇基因,他们的表达受到CDK7的转录调控,CDK7抑制,这些基因也异常敏感。 研究内容 第一部分:CDK7抑制剂(THZ1),选择性对三阴性乳腺癌发挥
三阴性乳腺癌是所有乳腺癌中最难治的一种类型之一,一直也没有寻找到特定的靶点。然而最新发表在Cell上一篇研究,对此有重大突破性发现,有望为三阴性乳腺癌的治疗开创新的时代(JEM:阻断CDK蛋白可导致三阴性乳腺癌萎缩 )。
CDK7是个跟细胞周期有关的蛋白激酶, THZ1是CDK7共价抑制剂。其实这个分子还有控制转录起始和延伸的作用。作者之前的团队报道过靶向CDK7的肿瘤治疗效应。
这篇文章是一个延续性研究,在三阴性乳腺癌,发现了那么一簇基因,他们的表达受到CDK7的转录调控,CDK7抑制,这些基因也异常敏感。
研究内容
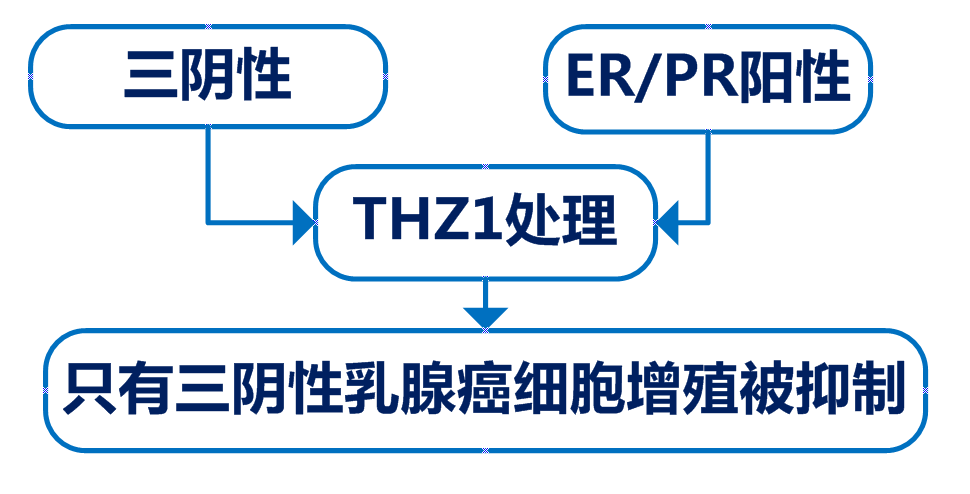
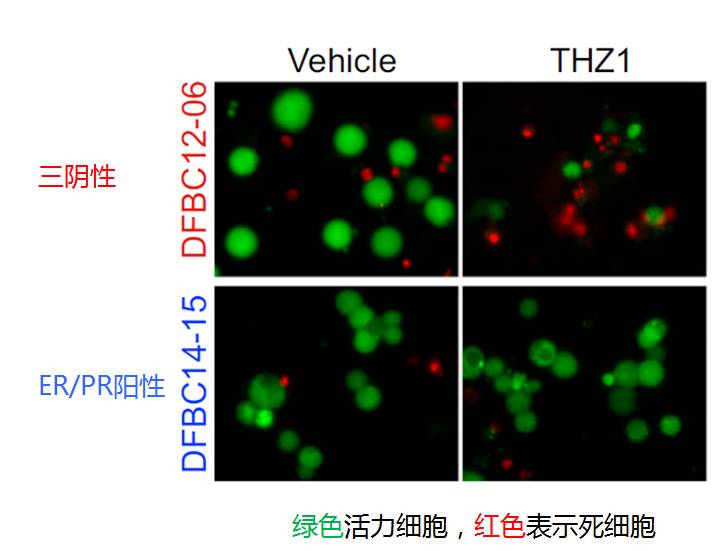
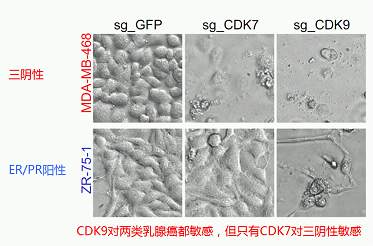
第一部分:CDK7抑制剂(THZ1),选择性对三阴性乳腺癌发挥抑制作用
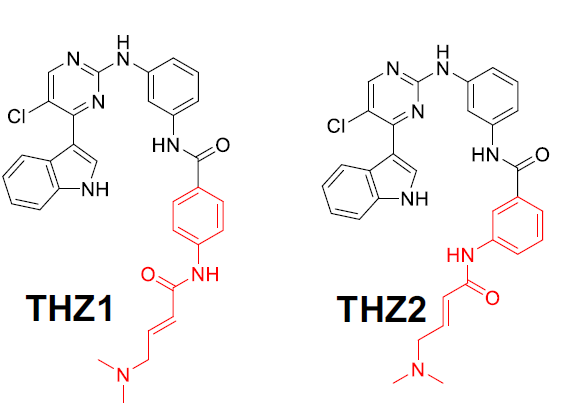
第二部分:合成THZ1的类似物THZ2(THZ1体内半衰期短),药效明显
第三部分:排除脱靶效应和家族其他分子的作用
用shRNA介导的基因沉默和CRISPR/Cas9介导的基因编辑,实现CDK7抑制,与化学抑制剂结果一致。

用CRISPR/Cas9技术分别抑制CDKs家族的6个分子:CDK7, 8, 9, 12, 13, 19。以上充分证实CDK7真真是三阴性乳腺癌治疗的好靶点!
第四部分:CDK7下游机制
作者去寻找那些在三阴性乳腺癌特异性高表达、对THZ1处理敏感、有超级增强子的成簇基因。锁定了8个分子。
利用CRISPR/Cas9技术把这8个基因分别敲除验证对三阴性乳腺癌增殖凋亡的关系。
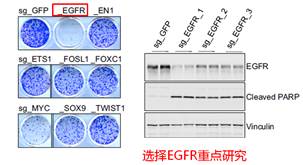
最后发现,现有的EGFR抑制剂对三阴性乳腺癌作用不显著,但用上CDK7抑制剂,肿瘤效果大大提升!
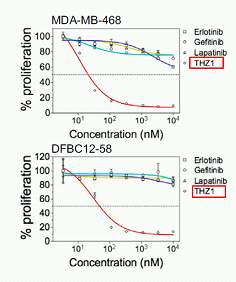
综上,本文介绍了CDK7介导的转录调控,对三阴性乳腺癌特异性的成簇基因,有重要的调节作用。抑制CDK7是这类难治性肿瘤的有效治疗手段。
原始出处:
Yubao Wang, Tinghu Zhang, Nicholas Kwiatkowski, Brian J. Abraham, Tong Ihn Lee, Shaozhen Xie, Haluk Yuzugullu, Thanh Von, Heyuan Li, Ziao Lin, Daniel G. Stover, Elgene Lim, Zhigang C. Wang, J. Dirk Iglehart, Richard A. Young, Nathanael S. Gray, Jean J. Zhao. CDK7-Dependent Transcriptional Addiction in Triple-Negative Breast Cancer. http://dx.doi.org/10.1016/j.cell.2015.08.063 In BriefSummaryFull-Text HTMLPDF
Nilson KA, Guo J, Turek ME, Brogie JE, Delaney E, Luse DS, Price DH.THZ1 Reveals Roles for Cdk7 in Co-transcriptional Capping and Pausing. Mol Cell. 2015 Aug 20;59(4):576-87
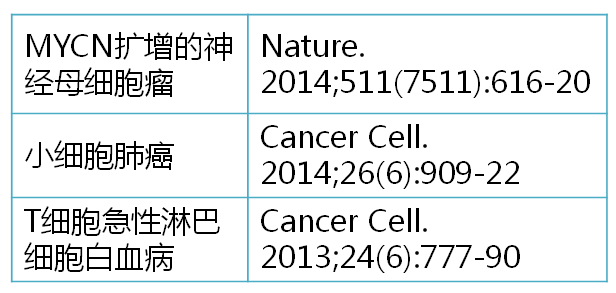
Chipumuro E, Marco E, Christensen CL, Kwiatkowski N, Zhang T, Hatheway CM, Abraham BJ, Sharma B, Yeung C, Altabef A, Perez-Atayde A, Wong KK, Yuan GC, Gray NS, Young RA, George RE.CDK7 inhibition suppresses super-enhancer-linked oncogenic transcription in MYCN-driven cancer. Cell. 2014 Nov 20;159(5):1126-39
Christensen CL, Kwiatkowski N, Abraham BJ, Carretero J, Al-Shahrour F, Zhang T, Chipumuro E, Herter-Sprie GS, Akbay EA, Altabef A, Zhang J, Shimamura T, Capelletti M, Reibel JB, Cavanaugh JD, Gao P, Liu Y, Michaelsen SR, Poulsen HS, Aref AR, Barbie DA, Bradner JE, George RE, Gray NS, Young RA, Wong KK.Targeting transcriptional addictions in small cell lung cancer with a covalent CDK7 inhibitor. Cancer Cell. 2014 Dec 8;26(6):909-22
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阴性乳腺癌#
30
#Cell#
31
#CEL#
32
很有实用性
114
#CDK#
34
#三阴性#
35