Cardiovasc Diabetol :他汀类药物强度、达到的低密度脂蛋白胆固醇水平和他汀类药物治疗时间对降低2型糖尿病患者心血管风险的相对贡献
2022-03-12 从医路漫漫 MedSci原创
2型糖尿病(T2D)常伴有血脂异常,其特征是甘油三酯(TG)升高,高密度脂蛋白胆固醇(HDL-C)降低,小而致密的低密度脂蛋白胆固醇(LDL-C)颗粒增多。
背景:2型糖尿病(T2D)常伴有血脂异常,其特征是甘油三酯(TG)升高,高密度脂蛋白胆固醇(HDL-C)降低,小而致密的低密度脂蛋白胆固醇(LDL-C)颗粒增多。先前的研究报道,用他汀类药物降低LDL-C可显著降低T2D患者动脉粥样硬化心血管事件的风险,因此,目前的血脂异常治疗指南一般建议成年T2D患者终生服用中强度或高强度的他汀类药物。
然而,关于他汀类药物的使用是否至关重要,或者获得的LDL-C浓度是否决定了动脉粥样硬化性心血管疾病的风险降低,仍存在争议。随机对照试验(RCT)提供的证据支持了所谓的他汀类药物和低密度脂蛋白胆固醇假说。然而,这些假设在以人口为基础的研究中往往是不可重现的,可能是由于难以控制的偏见所致。其中一个主要的偏向是在临床实践中不坚持使用他汀类药物。在荟萃分析中,新接受他汀类药物治疗的患者中有一半在一年内停止治疗。因此,在临床实践中,坚持使用他汀类药物对于解释他汀类药物对心血管的益处可能是至关重要的。我们注意到关于他汀类药物治疗持续时间的研究很少。此外,以往许多关于他汀类药物的随机对照试验的随访时间往往不够长,不足以观察他汀类药物的终生效应。此外,尽管对他汀类药物进行了大量试验,但针对T2D患者的研究寥寥无几。
目前的指南建议2型糖尿病(T2D)患者终生使用他汀类药物,然而,一些患者在临床实践中停止了他汀类药物的治疗。我们的目标是在真实环境中评估T2D患者的最佳他汀类药物治疗,包括他汀类药物治疗持续时间、他汀类药物强度和低密度脂蛋白胆固醇(LDL-C)水平。
方法:来自韩国国民健康保险服务队列(2007年-2015年)的8937例T2D患者,年龄≥40岁,接受他汀类药物治疗至少90天。根据他汀类药物强度、达到的血清低密度脂蛋白胆固醇水平和他汀类药物治疗时间,评估包括缺血性心脏病、缺血性中风和心血管死亡在内的主要心血管不良事件(MACE)的风险。通过计算各因素解释的对数似然比,量化这些因素对MACE风险的相对贡献。
结果:接受中、高强度他汀类药物治疗的患者发生MACE的风险比(HR)低于接受低强度他汀类药物治疗的患者(HR,0.72;p=0.027)。在接受中强度或高强度他汀类药物治疗的患者中,获得的低密度脂蛋白胆固醇水平与较低的心血管风险相关。值得注意的是,患者服用他汀类药物的时间越长,患MACE的风险就越低;作为治疗3-6个月的参考,MACE的心率在至少18个月后显著降低(调整后的HR为0.7;p=0.009)。他汀类药物持续时间(2.55)、低密度脂蛋白胆固醇水平(2.18)和他汀类药物强度(0.95)对MACE的可解释对数似然比最大。
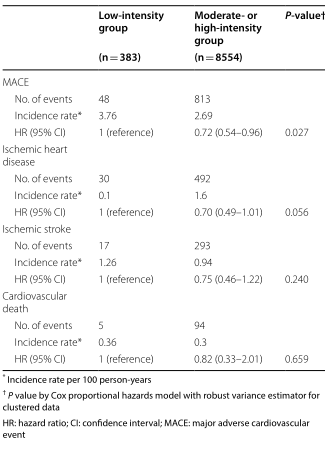
表1按他汀类药物用药强度划分的主要心血管事件累积发生率
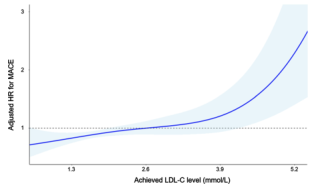
图1根据低密度脂蛋白胆固醇(LDL-C)水平(mmol/L)调整主要心血管事件危险比的三次样条曲线。根据正在治疗的LDL-C水平调整主要心血管事件的HR*(蓝线)和95%CI(阴影区域),参考2.6 mmol/L。95%CI达到参考线(HR=1)的点的LDL-C水平分别为1.9 mmol/L和4.2 mmol/L。*根据年龄、性别、社会经济状况、糖尿病病程、体重指数、空腹血糖、收缩压、肌酐、吸烟、饮酒、运动、既往心血管疾病(。和同时用药(抗血栓药物、抗高血压药物分类和抗糖尿病药物分类)
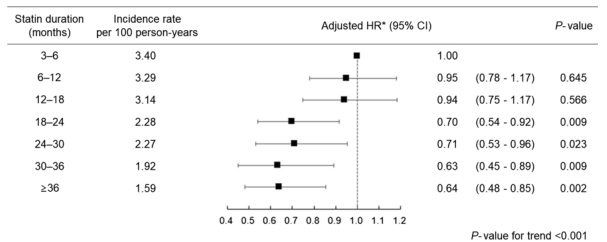
图2在接受中强度或高强度他汀类药物治疗的患者中,根据他汀类药物治疗时间的不同,发生主要心血管事件的风险。*根据年龄、性别、社会经济地位、糖尿病病程、体重指数、空腹血糖、收缩压、肌酐、吸烟、饮酒、锻炼、既有心血管疾病(缺血性心脏病、缺血性中风和心力衰竭)、同时服药(抗血栓药、抗高血压药分类和抗糖尿病药物分类)以及治疗前LDL-C水平进行调整
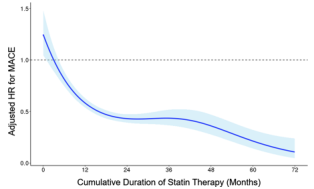
图3根据他汀类药物治疗时间调整主要心血管事件风险比的三次样条曲线。根据他汀类药物治疗3个月的时间计算主要心血管事件的调整HR*(实线)和95%CI(阴影区域)。*根据年龄、性别、社会经济地位、糖尿病病程、体重指数、空腹血糖、收缩压、肌酐、吸烟、饮酒、锻炼、既有心血管疾病(缺血性心脏病、缺血性中风和心力衰竭)以及同时服用药物(抗血栓药物、抗高血压药物分类和抗糖尿病药物分类)和治疗前LDL-C水平进行调整
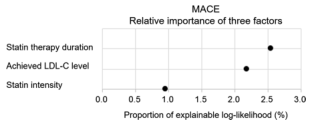
图4他汀类药物治疗持续时间、他汀类药物强度和达到的LDL-C水平作为MACE预测因子的相对重要性。通过计算每个危险因素解释的对数似然比,量化他汀类药物治疗时间、他汀类药物强度和达到的LDL-C水平的相对贡献。模型中的其他变量包括年龄、性别、社会经济状况、糖尿病病程、体重指数、空腹血糖、收缩压、肌酐、吸烟、饮酒、锻炼、既有心血管疾病(缺血性心脏病、缺血性中风和心力衰竭),以及同时服药(抗血栓药物、抗高血压药物分类和抗糖尿病药物分类)。他汀类药物治疗和糖尿病病程被包括为时间依赖变量。
结论:他汀类药物治疗时间与他汀类药物强度或达到的LDL-C水平一样重要,甚至比他汀类药物强度或达到的LDL-C水平更重要,对降低T2D患者的心血管风险同样重要。在临床实践中应考虑“越长越好”的他汀类药物治疗理念。
原文出处:Kim JY, Choi J, Kim SG,et al.Relative contributions of statin intensity, achieved low-density lipoprotein cholesterol level, and statin therapy duration to cardiovascular risk reduction in patients with type 2 diabetes: population based cohort study.Cardiovasc Diabetol 2022 Feb 22;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
37
#治疗时间#
34
#ASC#
41
#血管风险#
51
#他汀类药#
50
#DIA#
33
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
37
好的
46
学习
53
好文章,谢谢分享。
53