骨折修复术-骨折分类、手术方法、手术过程和手术预后(图片)
2015-12-03 网络 MedSci原创
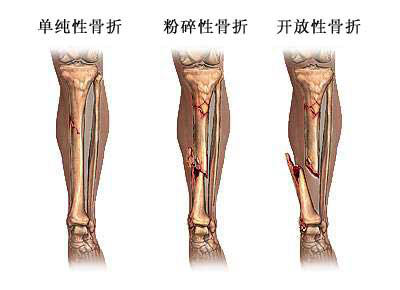
骨折的分类多种多样:单纯性骨折的骨头只有一条骨折线;粉碎性骨折的骨头碎裂成两块以上;开放性骨折的骨头刺破皮肤,骨折处与外界相通。 病人全麻或局麻,手术切口位于骨折区域。术中将骨骼复位,根据实际情况把接骨板、螺丝钉、髓内钉、加压钢板暂时或永久性地安装在骨骼里,固定骨骼。 结扎或电凝断骨折区断裂的血管。如果有大量骨骼缺失,特别是骨与骨之间出现较大的缺口,可考虑进行骨移植,以便病人能更快地康

骨折的分类多种多样:单纯性骨折的骨头只有一条骨折线;粉碎性骨折的骨头碎裂成两块以上;开放性骨折的骨头刺破皮肤,骨折处与外界相通。

骨折修复术的三个主要方法是:
*石膏绷带固定
*手术复位与内固定:是施行手术,切开骨折部的软组织,暴露骨折段,在直视下将骨折复位。复位后,可以用对人体组织无不良反应的金属内固定物,如接骨板、螺丝钉、髓内钉、加压钢板等,也可用自体或异体植骨片,将骨折段固定。
*手术复位与外固定:是施行手术,将骨折复位,并在骨折的肢体外安装骨外固定器。骨外固定器是一个由夹头和钢管组装成的体外钢架,可以支持骨骼,矫正骨骼在愈合过程中出现的各种移位。这种固定方法普遍适用于不能用内固定术的复杂骨折。

病人全麻或局麻,手术切口位于骨折区域。术中将骨骼复位,根据实际情况把接骨板、螺丝钉、髓内钉、加压钢板暂时或永久性地安装在骨骼里,固定骨骼。
结扎或电凝断骨折区断裂的血管。如果有大量骨骼缺失,特别是骨与骨之间出现较大的缺口,可考虑进行骨移植,以便病人能更快地康复。若不进行骨移植,也可用以下的方法固定骨骼:
1)在骨骼中插入多根骨钉;
2)用接骨板加螺丝钉内固定;
3)在骨骼中插入长条状的髓内钉。
个别病例,手术固定骨骼后,还要进行显微外科手术修复受损的血管和神经。术后常规缝合皮肤。

内固定术后病人康复较快,预后好。如果内固定装置在体内不出现问题,可长期留在人体内。
术后住院时间由骨骼愈合情况、有无感染、血管神经供应、有无合并其他外伤等因素决定。儿童骨折愈合较快,通常在6周内可以康复。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#修复术#
42
不错,赞一个
89
这篇文章有一定深度
58
是一篇不错的文章
132
非常实用
131
好文章,值得收藏
121
#手术方法#
48