Ann Hematol:血液系统恶性肿瘤患者的体外膜肺氧合:系统评价和荟萃分析
2022-05-30 网络 网络
与其他ECMO适应症相比,需要ECMO的HM患者的生存率相对较差。预后较差风险的患者包括年龄较大、男性和HSCT接受者
由于出血和感染并发症,血液系统恶性肿瘤 (HM) 一直被视为体外膜肺氧合 (ECMO) 的禁忌证。然而,关于是否应将 ECMO 用于 HM 患者的相互矛盾的文献仍然存在。一研究团队进行了一项随机效应荟萃分析,以调查 HM 患者对 ECMO 的结果。
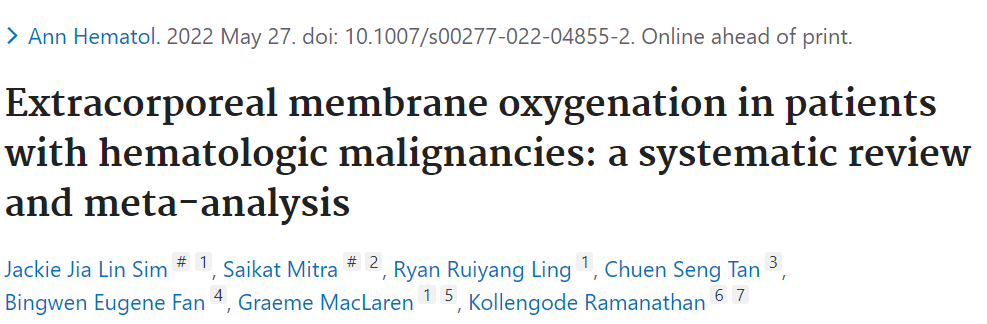
他们在2021年10月10日之前搜索了Medline、Embase、Scopus和Cochrane。使用JBI清单和GRADE方法分别评估证据的偏倚风险和确定性。纳入了 13 项观察性研究(422 名 HM 患者,9778 名无 HM 对照)。HM患者和那些为HM需要ECMO的适应症而进行造血干细胞移植的患者的综合住院死亡率分别为79.1% (95%CI: 70.2-86.9%)和87.7% (95%CI: 80.4-93.8%)。
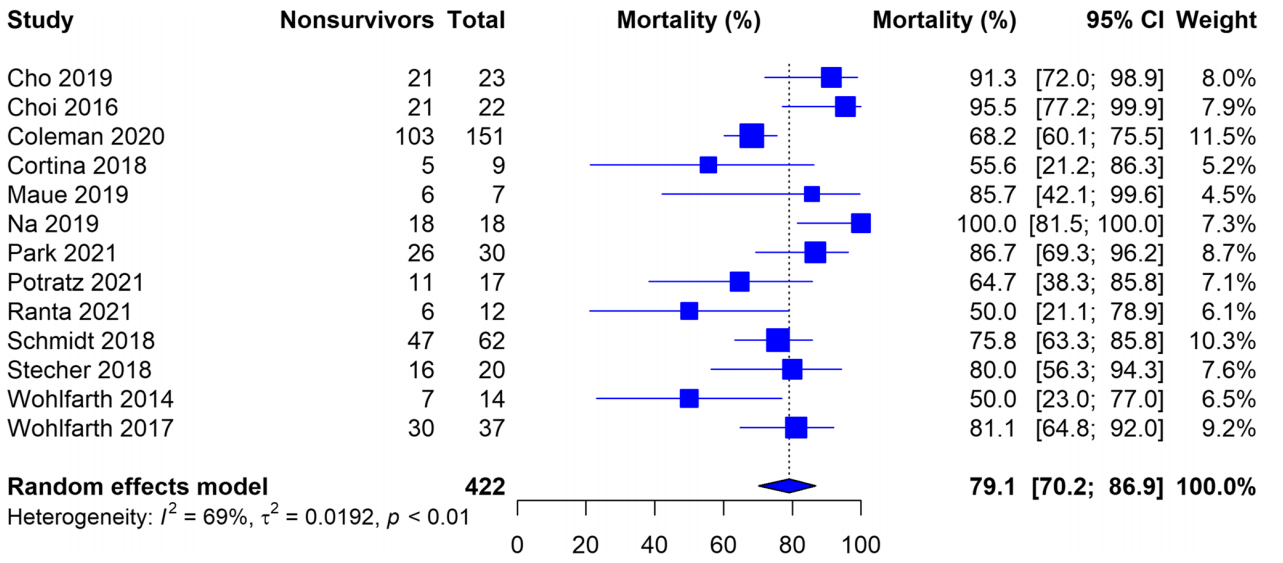
图1:采用体外膜氧合法合并恶性血液病患者的住院死亡率
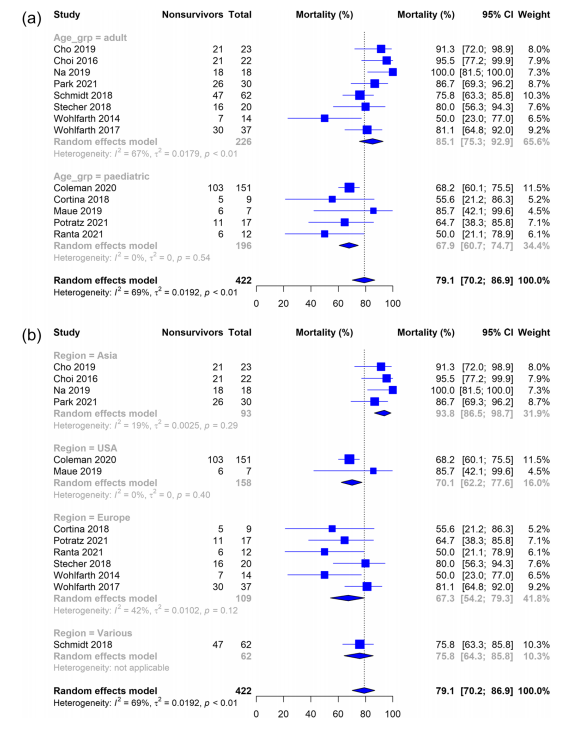
图2:a 年龄(成人vs儿童)、b 地理区域(亚洲vs北美和欧洲)和c 造血干细胞移植患者的亚组分析
亚组分析发现,成人死亡率高于儿童(85.1% vs 67.9%,p= 0.003),亚洲高于北美和欧洲(93.8% vs 69.6%,p< 0.001)。合并 ECMO 持续时间为 10.0 天(95%CI:7.5-12.5);合并 ICU 和住院时间分别为 19.8 天(95%CI:12.4-27.3)和 43.9 天(95%CI:29.4-58.4)。年龄(回归系数[B]:0.008,95%CI:0.003-0.014),男性比例(B:1.799,95%CI:0.079-3.519),ECMO持续时间(B:- 0.022,95%CI:- 0.043 至 - 0.001)与较高的死亡率显着相关。
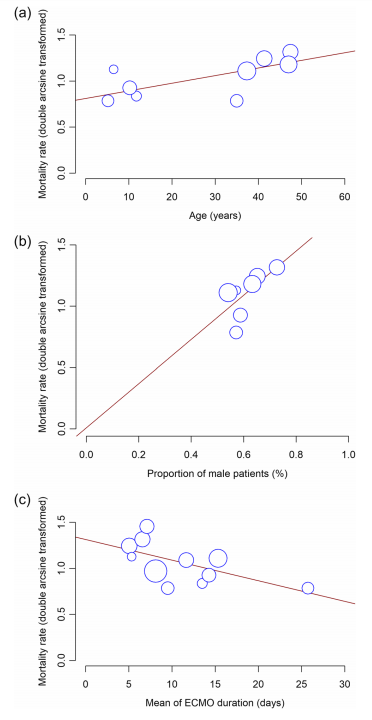
图3:平均年龄、男性患者比例b、c体外膜氧合持续时间平均值与住院死亡率的meta回归的气泡图
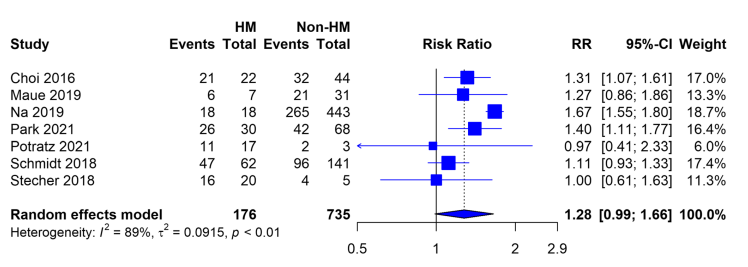
图4:血液系统恶性肿瘤患者与非恶性血液病患者体外膜氧合的死亡率风险比
在北美和欧洲,需要ECMO的HM患者的住院死亡率为79.1%,儿童预后更好。ECMO不应被视为这些患者的常规支持治疗,但可以根据具体情况仔细考虑。
总的来说,与其他ECMO适应症相比,需要ECMO的HM患者的生存率相对较差。预后较差风险的患者包括年龄较大、男性和HSCT接受者。考虑到该队列在使用ECMO时死亡率较高,应根据每个患者明智地考虑体外治疗。未来的研究应集中于探索ECMO启动的理想时间,并试图为这些患者建立特异性的启动标准。
原始出处:
Sim JJL, Mitra S, Ling RR, Tan CS, Fan BE, MacLaren G, Ramanathan K. Extracorporeal membrane oxygenation in patients with hematologic malignancies: a systematic review and meta-analysis. Ann Hematol. 2022 May 27. doi: 10.1007/s00277-022-04855-2. Epub ahead of print. PMID: 35622097.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#荟萃分析#
53
#血液系统#
0
#荟萃#
37
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
40
#血液系统恶性肿瘤#
42
#EMA#
31
#肿瘤患者#
31
#评价#
39