PNAS:免疫系统可能在阿尔茨海默病中发挥比想象中更大的作用
2016-03-03 佚名 生物谷
在最近发表于《Proceedings of the National Academy of Sciences》期刊的研究中,加州大学欧文分校、Sue & Bill Gross干细胞研究中心(Sue & Bill Gross Stem Cell Research Center)以及记忆障碍和神经系统疾病研究所的神经生物学家们发现,通常帮助我们对抗细菌和病毒感染的免疫细胞,可能在阿尔茨
在最近发表于《Proceedings of the National Academy of Sciences》期刊的研究中,加州大学欧文分校、Sue & Bill Gross干细胞研究中心(Sue & Bill Gross Stem Cell Research Center)以及记忆障碍和神经系统疾病研究所的神经生物学家们发现,通常帮助我们对抗细菌和病毒感染的免疫细胞,可能在阿尔茨海默病中发挥比最初认为的更大的作用。
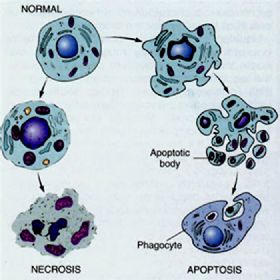
研究人员发现,当阿尔茨海默病小鼠的血液中缺失这些关键免疫细胞,它们会更快地发展出与阿尔茨海默病相关的独特大脑斑块。
神经生物学与行为助理教授Mathew Blurton-Jones和博士生Samuel Marsh表示,他们的发现可能导向对新技术的创建,以帮助识别、甚至可能治疗面临该病风险的个人。
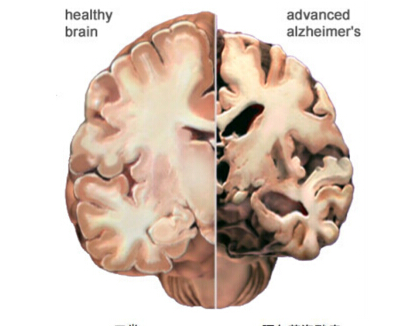
阿尔茨海默病是老年性痴呆的主要原因,被认为是由一种蛋白质的积聚所驱动的。这种蛋白质被称为β-淀粉样蛋白,会在大脑中聚合形成淀粉样蛋白斑块。大脑内部的小胶质细胞会试图清理这种积累,但在阿尔茨海默病中,它们似乎是在打一场注定会失败的战争。虽然许多研究已经探索了小胶质细胞在阿尔茨海默病的作用,但很少有研究人员探究T-细胞和B-细胞的作用。这些免疫细胞驻留在大脑之外,在自身免疫疾病中扮演重要角色,也会影响阿尔茨海默病。
为了测试这个想法,Blurton-Jones和Marsh培育了缺失3种关键免疫细胞(T-细胞、B-细胞和NK-细胞)的转基因阿尔茨海默病小鼠。6个月后,这些小鼠大脑中的β-淀粉样蛋白积聚是拥有完好免疫系统的阿尔茨海默病小鼠的两倍以上。
"影响的程度之大让我们非常惊讶"Blurton-Jones说,"我们预期的免疫系统缺陷对阿尔茨海默病病理的影响要微弱得多。"
为了理解这些免疫细胞缺失如何增加β-淀粉样蛋白,他和Marsh研究了这些外围细胞和大脑中小胶质细胞之间的相互作用。
"我们发现,在拥有完好免疫系统的阿尔茨海默病小鼠中,B-细胞制造的抗体会在大脑中积聚并与小胶质细胞相关联。这有助于增加对β-淀粉样蛋白的清理"Marsh说。
为了进一步证实血液中免疫细胞与大脑中免疫细胞之间相互作用的重要性,研究人员将健康的骨髓干细胞植入存在免疫缺损的阿尔茨海默病小鼠体内。由于T-细胞、B-细胞和NK-细胞发育自骨髓干细胞,移植导向缺失免疫细胞的再造。这使得B-细胞产生抗体,再次抵达大脑并辅助小胶质细胞消除β-淀粉样蛋白。
"我们知道,免疫系统会随着年龄增长而发生变化,制造T-细胞和B-细胞的能力会下降"Blurton-Jones说,"所以,人类免疫系统的衰老是否会促使阿尔茨海默病的发展是我们想要探究的下一个重大问题。"
原始出处:
Samuel E. Marsha,Edsel M. Abuda,b,Anita Lakatos,et al.The adaptive immune system restrains Alzheimer's disease pathogenesis by modulating microglial function.PNAS,19 January 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#阿尔茨#
19
#阿尔茨海#
22
#PNAS#
21
#阿尔茨海默#
33
嗯
97