J Autoimmun:皮肤CD4+Trm细胞区分急性皮肤红斑狼疮和局限性盘状红斑狼疮/亚急性皮肤红斑狼疮及其他皮肤病
2022-03-21 医路坦克 MedSci原创
本文分析和比较急性CLE、亚急性CLE和局限性盘状红斑狼疮皮损患者外周血中经SMART RNA测序(SMART-SEQ)鉴定的CD4+Trm细胞和黑色素瘤中缺失的AIM2细胞。
皮肤红斑狼疮(CLE)是一种自身免疫性疾病,表现为局限性皮肤病或皮肤表现,出现在70%-80%的系统性红斑狼疮(SLE)患者。CLE特异性皮肤损害可细分为急性CLE(ALE)、亚急性CLE(SCLE)和慢性CLE(CCLE)。主要的CCLE变异型是慢性盘状红斑狼疮(CDLE),又可细分为局限性DLE(局限性DLE:影响头部和面部皮肤)或播散性DLE(播散性DLE:影响颈部上方和下方皮肤)。器官受累的发生率在不同亚型的CLE患者中不同。值得注意的是,ALE的全身受累发生率最高(90%),而局限性DLE造成的损害总是局限于皮肤。
在系统性红斑狼疮患者中,皮肤表现的利妥昔单抗反应在不同的皮损类型中是不同的。具体地说,在ALE患者中,抗B细胞疗法可以改善皮肤病的状况,而SCLE和CCLE患者对B细胞耗尽的反应较差。令人惊讶的是,在几名患有或没有皮肤病的患者中观察到了SCLE和CCLE的出现,而其他器官系统同时对利妥昔单抗治疗反应良好。因此,ACLE可能与B细胞信号和异常的CD4+T滤泡辅助细胞有更强的相关性,这些细胞可以诱导各种自身抗体的产生。Abatacept抑制T细胞激活,对一些难治性SLE患者有益,但会加重难治性SLE患者的DLE病变。CLE皮肤病变中的Trm细胞可能为不同CLE亚型之间的免疫病理差异提供了解释。
问题驻留记忆T(Trm)细胞由CD69和/或CD103的表达定义,永久驻留在皮肤中,并迅速触发同源病原体衍生的局部炎症反应。到目前为止,存在于不同组织中的记忆T细胞在保护或病理过程中显示出组织特异性。由于Trm细胞寿命长,对破坏因素具有抵抗力,并具有持续的促炎优势,不适当的Trm细胞激活可能会导致免疫病理和同一部位的疾病持续时间延长,为了完全缓解疾病,需要设计出完全沉默Trm细胞的最佳治疗方案。
在这项研究中,我们使用Smart-Seq分析了NCS和ALE患者皮肤中CD4+Trm细胞的基因表达谱。此外,采用免疫组织化学方法检测了局限性DLE、SCLE、ALE等炎症性皮肤病皮损中CD4+Trm细胞的数量和分布。我们的数据显示,来自NCS和ALE患者的CD4+Trm细胞具有不同的转录特性。多色免疫组织化学显示,与NCS相比,局限性DLE和SCLE患者的CD4+Trm细胞数量增加,但Acle患者的CD4+Trm细胞数量没有增加。
我们用Smart-Seq研究了ALE患者和正常对照(NCS)真皮中CD4+Trm细胞的差异。应用多色免疫组织化学方法检测134例临床患者,包括局限性DLE(n=19)、ALE(n=19)、SCLE(n=16)、银屑病(n=12)、酒渣鼻(n=17)、扁平苔藓(n=18)、环状肉芽肿(n=15)和NCS(n=18)皮肤中CD4+Trm细胞的AIM2水平。
Smart-Seq检测显示AIM2在ALE皮损的皮肤CD4+Trm细胞中的表达高于NCS(倍数变化>10,调整后P<0.05)。AIM2在CD4+Trm细胞中的表达不受年龄和性别的影响。ALE患者外周血中AIM2的表达显著低于局限性DLE(179.41±160.98)和SCLE(63.43±62.27,P<0.0001)。在ALE与局限性DLE和SCLE的总体比较中,AIM2表达的受试者操作特征曲线在截断值为18.26时的敏感性为100.00%,特异性为82.86%。ALE与局限性DLE比较,敏感性为89.47%,特异性为100.00%(以12.26为界值)。ALE与SCLE比较,敏感性为100.00%,特异度为75.00%,界值为18.26。
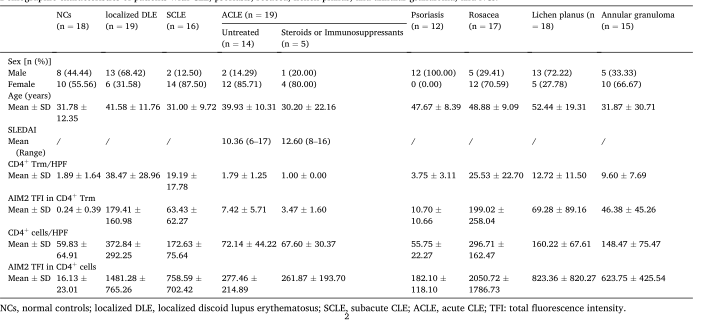
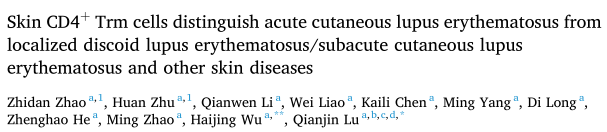
表1 CLE、银屑病、酒渣鼻、扁平苔藓、环状肉芽肿和NCS患者的人口学特征。

图1. 来自ALE患者的皮肤CD4?Trm细胞与NCS相比显示出不同的转录组表达谱。(1)从ACLE和NCS患者的皮肤中分离出CD4+Trm细胞。(B)散点图,显示Acle CD4+Trm细胞(y轴)和正常CD4+Trm细胞(x轴)之间基因表达的差异。然后对这些值进行平均,以获得每个组的归一化信号值(按对数2标度)。(C)通过KEGG分析对差异表达基因(Deg)进行分类。(D)通过GO分析对差异表达基因(DEG)进行分类。
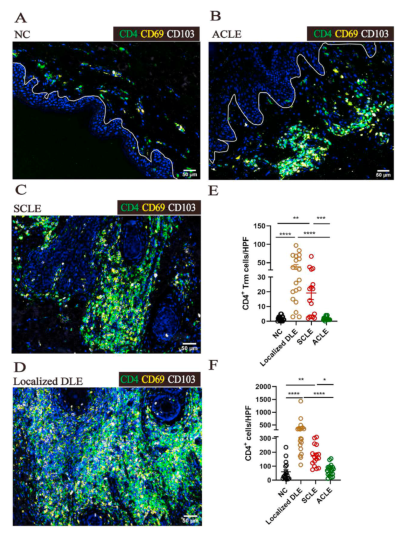
图2. 皮肤CD4+Trm细胞在NCS、ALE、SCLE和局限性DLE患者中的数量和分布。(A-D)免疫组织化学染色在NCS、ALE、SCLE和局限性DLE患者的石蜡切片中。CD4(绿色)、CD69(黄色)、CD103(白色)。(E)比较NCS(n=18)、局限性DLE(n=19)、Acle(n=19)和SCLE(n=16)患者的CD4+Trm细胞。(F)NCS(n=18)与局限性DLE(n=19)、Acle(n=19)和SCLE(n=16)患者的CD4+细胞比较。**P<0.001,*P<0.0001;Kruskal-Wallis检验和Dunn‘s多重后置检验。
图3.7例炎症性皮肤病患者皮肤中CD4+Trm细胞的数量和分布。(A)Acle、SCLE、局限性DLE、牛皮癣、酒渣鼻、扁平苔藓和环状肉芽肿患者石蜡切片中的多重免疫组织化学染色。CD4(绿色)、CD69(黄色)、CD103(白色)。(2)ALE患者(n=19)与银屑病(n=12)、酒渣鼻(n=17)、扁平苔藓(n=18)、环状肉芽肿(n=15)患者外周血中CD4+Trm细胞的比较。(C)系统性红斑狼疮患者(n=16)与银屑病患者(n=12)、酒渣鼻患者(n=17)、扁平苔藓患者(n=18)、环状肉芽肿患者(n=15)外周血中CD4+Trm细胞的比较。(D)局限性DLE患者(n=18)与银屑病患者(n=12)、酒渣鼻患者(n=17)、扁平苔藓患者(n=18)、环状肉芽肿患者(n=15)外周血中CD4+Trm细胞的比较。**P<0.001,*P<0.0001;Kruskal-Wallis检验和Dunn‘s多重后置检验。
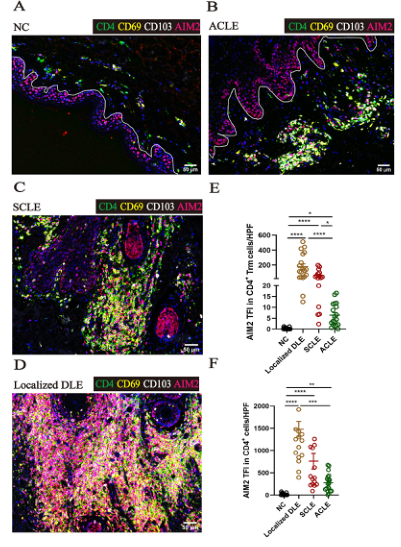
图4. AIM2在NCS、ALE、SCLE、DLE患者外周血中的表达。(A-D)免疫组织化学染色在NCS、ALE、SCLE和局限性DLE患者的石蜡切片中。CD4(绿色)、CD69(黄色)、CD103(白色)、AIM2(红色)。(E)比较NCS(n=18)、局限性DLE(n=19)、Acle(n=19)和SCLE(n=16)患者外周血中CD4+Trm细胞AIM2总荧光强度(TFI)。(F)比较NCS(n=18)、局限性DLE(n=19)、Acle(n=19)和SCLE(n=16)患者的CD4+细胞AIM2 TFI。**P<0.001,*P<0.0001;Kruskal-Wallis检验和Dunn‘s多重后置检验。

图5. 7例炎症性皮肤病患者CD4+Trm细胞中AIM2的表达。(A)Acle、SCLE、局限性DLE、牛皮癣、酒渣鼻、扁平苔藓和环状肉芽肿患者石蜡切片中的多重免疫组织化学染色。CD4(绿色)、CD69(黄色)、CD103(白色)、AIM2(红色)。(B)ALE患者(n=19)与银屑病(n=12)、酒渣鼻(n=17)、扁平苔藓(n=18)、环状肉芽肿(n=15)患者外周血CD4+Trm细胞AIM2 TFI的比较。(C)SCLE患者(n=16)与银屑病患者(n=12)、酒渣鼻患者(n=17)、扁平苔藓患者(n=18)、环状肉芽肿患者(n=15)的CD4+Trm细胞AIM2 TFI的比较。(D)比较局限性DLE(n=19)、银屑病(n=12)、酒渣鼻(n=17)、扁平苔藓(n=18)和环状肉芽肿(n=15)患者外周血中CD4+Trm细胞的AIM2 TFI。**P<0.001,*P<0.0001;Kruskal-Wallis检验和Dunn‘s多重后置检验。
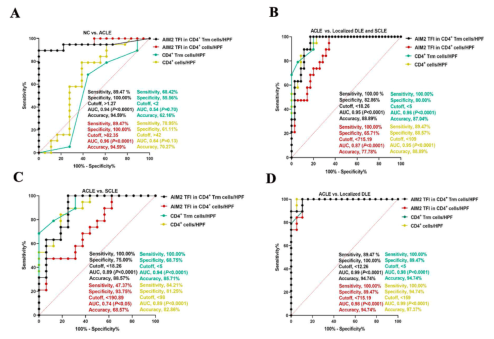
图6. 基于皮肤CD4+细胞的ROC曲线,CD4+细胞的AIM2 TFI,CD4+Trm细胞的AIM2 TFI和CD4+Trm细胞的AIM2 TFI。(A)ALE患者与NCS患者的ROC曲线比较。(B)ALE患者与局限性DLE和SCLE患者的ROC曲线比较。(C)ALE患者与SCLE患者的ROC曲线比较。(D)ALE患者与局限性DLE患者的ROC曲线比较。**P<0.001,*P<0.0001;
与ALE相比,在SCLE和局限性DLE的皮损中,CD4+Trm细胞的数量增加,提示在SCLE和局限性DLE的持续性皮损中,CD4+Trm细胞可能起着更重要的作用。此外,AIM2在CD4+Trm细胞中的表达可将ALE患者与局限性DLE和SCLE患者区分开来。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#皮肤病#
49
#CD4#
38
#CD4+#
34
#局限性#
29
学习了
52
#狼疮#
36
#红斑#
30