Heart:特发性慢性大面积心包积液的结局分析
2018-10-02 xing.T MedSci原创
由此可见,“特发性”慢性大面积心包积液的演变通常是良性的,大多数病例的积液量有所减少,约40%的病例积液消退。心脏压塞的风险为2.2%/年,并且在没有干预的情况下保守治疗患者的无复发/并发症存活期更好。
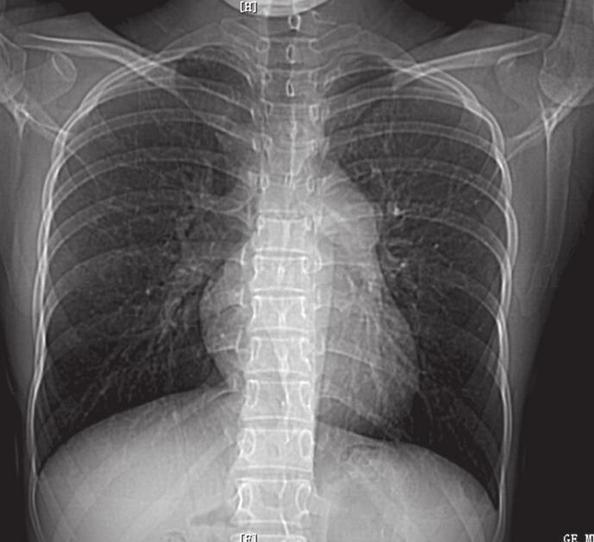
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究的目的是评估“特发性”慢性大面积心包积液的结局,这些患者没有心包炎的初步证据。
在一项前瞻性队列研究中,研究人员纳入了2000年至2015年期间在意大利三个心包疾病转诊中心评估的特发性慢性大面积心包积液的所有病例。术语“特发性”适用于进行完整诊断评估以排除特定病因的病例。每3-6个月进行一次临床和超声心动图随访。
该研究纳入的100例患者(平均年龄为61.3±14.6岁,54例女性,44例患者根据临床评估无症状),平均随访50个月。心包积液的基线中位数(评估指标为最大舒张末期无回声空间)为25 mm(IQR为8),在随访结束时39例患者积液完全消退平均值降至7 mm(IQR为19; p<0.0001)。没有新的病因诊断。不良事件分别为:心脏压塞8例(8.0%),心包穿刺30例(30.0%),心包窗12例(12.0%)和心包切除3例(3.0%)。未经干预措施的患者无复发生存期和无并发症生存期更好(对数秩p=0.0038)。
由此可见,“特发性”慢性大面积心包积液的演变通常是良性的,大多数病例的积液量有所减少,约40%的病例积液消退。心脏压塞的风险为2.2%/年,并且在没有干预的情况下保守治疗患者的无复发/并发症存活期更好。
原始出处:
Massimo Imazio.et al.Outcomes of idiopathic chronic large pericardial effusion.Heart. 2018. http://dx.doi.org/10.1136/heartjnl-2018-313532
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#大面积#
29
#特发性#
32
#心包积液#
51
#ART#
32
#HEART#
27
学习了
70
很好
66
不错的文章值得拥有哦
73
了解一下,谢谢分享!
57