Am Heart J:佐他莫司洗脱支架抗再狭窄效果更佳
2012-11-27 高晓方译 医学论坛网
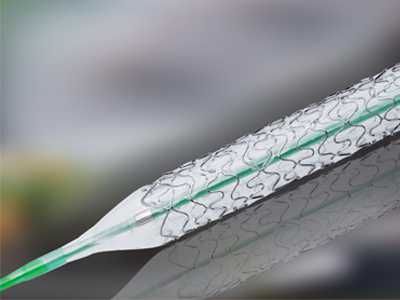
德国学者的一项研究表明,Resolute佐他莫司洗脱支架(R-ZES)的抗再狭窄效果优于Endeavor佐他莫司洗脱支架(Z-ZES)。论文于2012年11月21日在线发表于《美国心脏杂志》(Am Heart J)。 R-ZES和Z-ZES采用了相同的金属平台和抗再狭窄药物,但前者包被有可增强药物释放的生物相容性聚合物。此项研究分别纳入了1000例和339例接受R-Z
德国学者的一项研究表明,Resolute佐他莫司洗脱支架(R-ZES)的抗再狭窄效果优于Endeavor佐他莫司洗脱支架(Z-ZES)。论文于2012年11月21日在线发表于《美国心脏杂志》(Am Heart J)。
R-ZES和Z-ZES采用了相同的金属平台和抗再狭窄药物,但前者包被有可增强药物释放的生物相容性聚合物。此项研究分别纳入了1000例和339例接受R-ZES和Z-ZES治疗的患者。有效性终点为目标病变血运重建,安全性终点则由目标血管相关性心源性死亡或心梗发生率以及随访2年时确定性支架血栓形成发生率所组成。
结果显示,2年时R-ZES组和Z-ZES组目标病变血运重建发生率分别为12.0%和16.0%[危险比(HR)0.72;P=0.052]。两组患者的心源性死亡或心梗发生率分别为5.5%和4.8%,明确支架血栓形成发生率分别为0.4%和0.6%。血管造影再狭窄的所有指标均有利于R-ZES;R-ZES组和Z-ZES组支架内晚期管腔丧失分别为0.29±0.56和0.58 ±0.55(P<0.0001)。
链接:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#洗脱支架#
46
#ART#
30
#再狭窄#
33
#HEART#
20