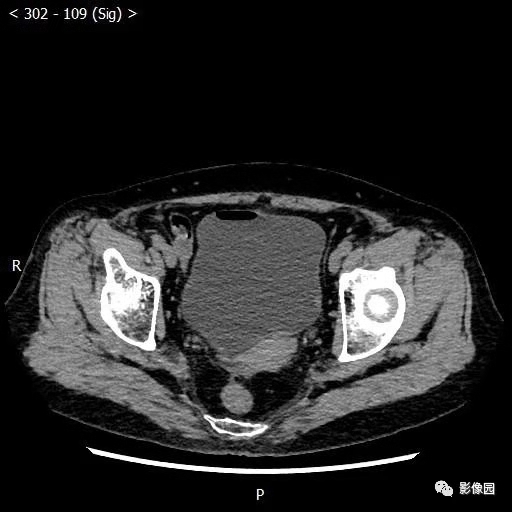
Cell Physiol Biochem:在膀胱癌细胞中,miR-1-3p能够促进细胞增殖和入侵
2018-11-30 AlexYang MedSci原创
越来越多的证据表明miR-1-3p在恶性肿瘤的恶化过程中具有重要作用。然而,miR-1-3p在膀胱癌中的特异生物学功能仍旧未知。研究人员通过qRT-PCR对膀胱癌组织和细胞系的miR-1-3p水平进行了调查,并利用亚硫酸盐测序PCR进行DNA甲基化分析;利用双荧光素酶报告实验确定了miR-1-3p靶标,并在体内和体外试验中调查了miR-1-3p对膀胱癌细胞的表型影响。研究发现,miR-1-3p在膀
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
0
#miR#
37
#Bio#
47
#Physio#
39
#Cell#
50
#癌细胞#
34
#细胞增殖#
30