JAMA Oncol:脑洞大开:CT扫描肌肉和脂肪可预测非转移性乳腺癌患者生存
2018-04-30 Jenny 肿瘤资讯
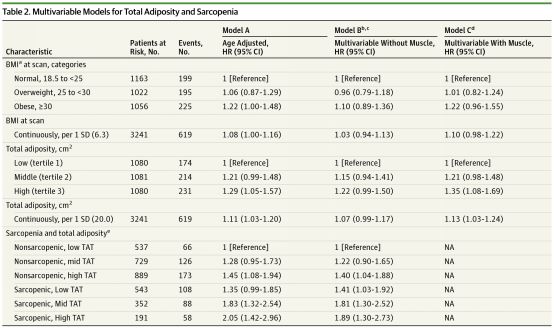
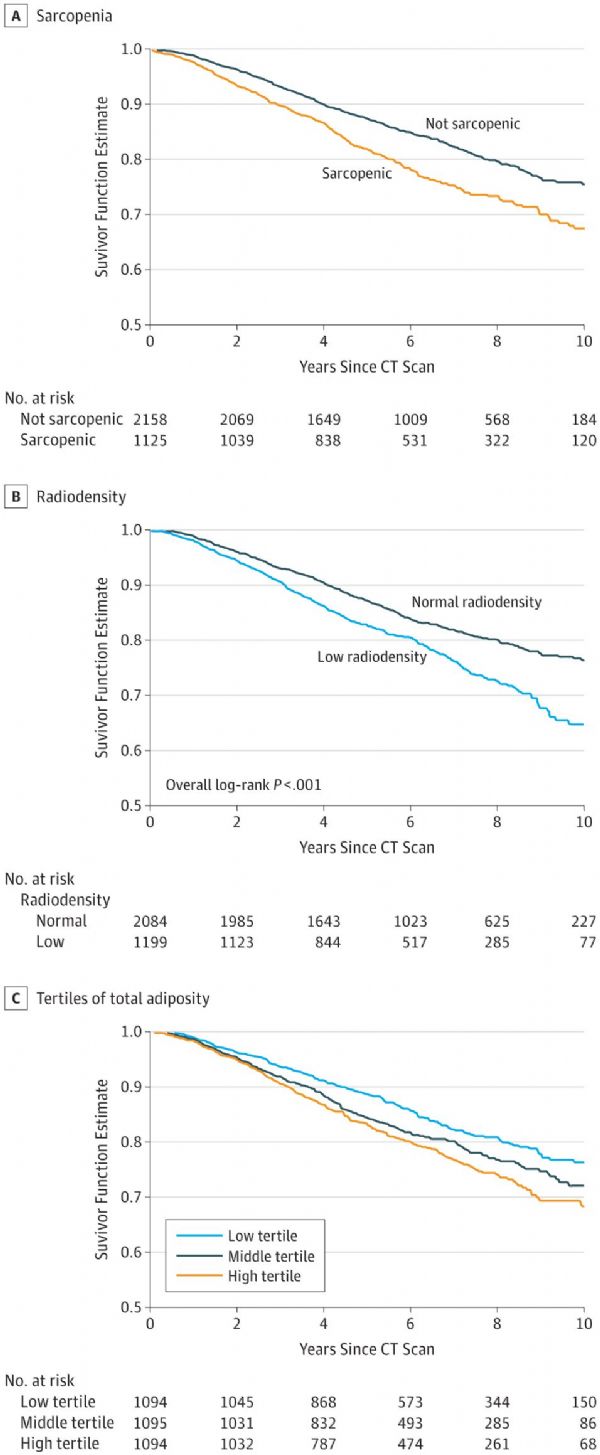
肿瘤患者过瘦或肥胖均可能增加死亡风险,但却有一种特殊情况,即BMI正常,但却是个瘦胖子(脂肪过多)或是胖瘦子(肌肉过少)。《JAMA Oncology》2018年4月5日在线发表一项研究,通过CT检测身体成分肌肉和脂肪与非转移性乳腺癌患者生存的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非转移#
29
#患者生存#
25
#Oncol#
32
#非转移性#
32
#脑洞大开#
0
学习了
57
#转移性#
29
#乳腺癌患者#
29
#CT扫描#
26
对于初学者非常好.学习了.谢谢老师
60