胃食管反流病(GERD)是指胃、十二指肠内容物反流入食管引起临床症状和(或)食管黏膜损伤的一种疾病,其主要表现为反酸、烧心或食物反流等症状。
反流物主要包括胃酸、胃蛋白酶,还有十二指肠液、胆酸、胰液等,其中胃酸和胃蛋白酶在临床上多见,而十二指肠液多见于胃大部切除术后、胃肠吻合术后、食管肠吻合术后。
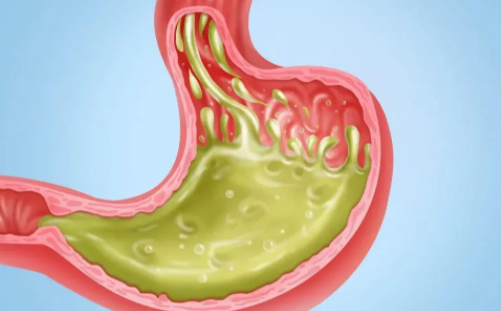
01 发病机制
据数据显示,GERD在世界范围内的患病率为13.3%,我国GERD患病率为为2.5% ~ 7.8%,低于欧美国家,但有上升趋势,并与韩国和日本接近。在年龄50岁、吸烟、使用非甾 体抗炎药/阿司匹林和肥胖患者中,GERD患病率更高。
虽然GERD与胃酸有关,但并不意味着这类患者的胃酸分泌过高,而是胃酸所处部位异常,即胃酸从胃反流至食管,使食管暴露于胃酸时间过长,从而引起临床症状和(或)食管黏膜损伤。
2019年发布的《中国胃食管反流病多学科诊疗共识》指出,多种因素和多个部位均参与了GERD的发生,而以胃食管交界区(GEJ)为GERD发生的初始部位,也是导致反流的最主要的解剖部位。
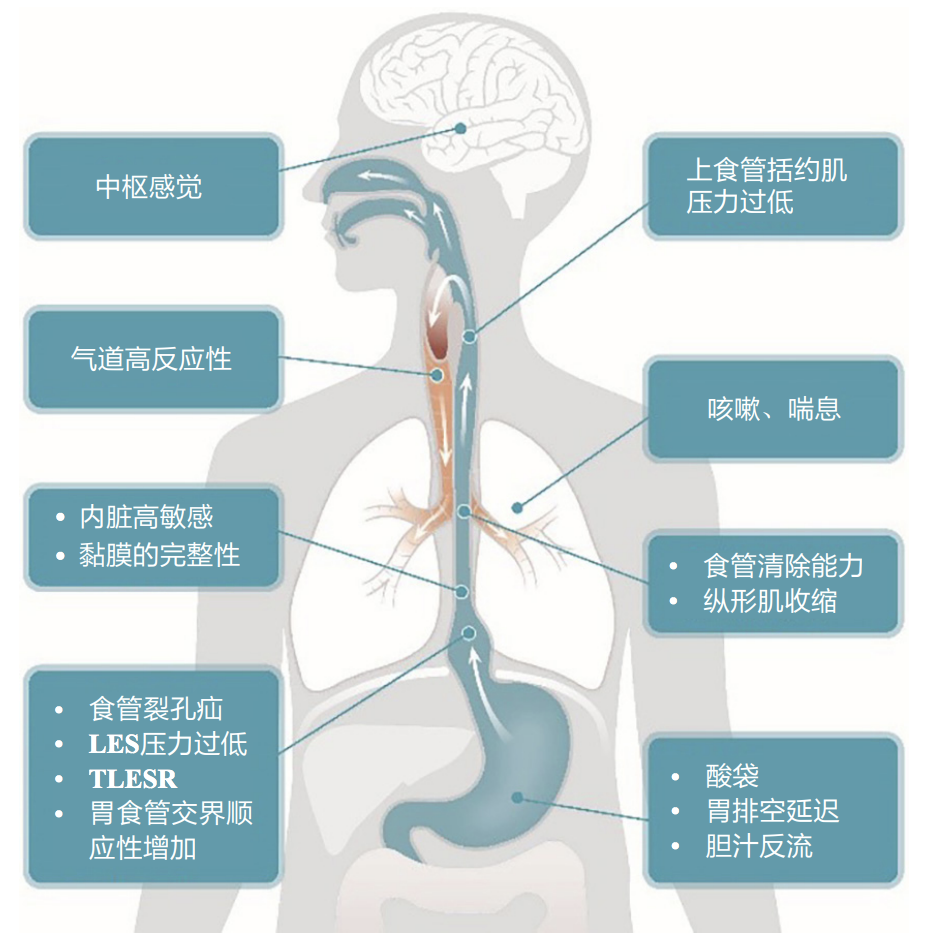
图:GERD的发病机制
GEJ由多个结构构成其抗反流功能,比如下食管括约肌(LES)的顺应性和产生的腔内压力、膈肌脚(食管裂孔)的顺应性和产生的腔外压力、膈食管膜的完整性(将下食管固定于膈裂孔)、腹段食管、腹段食管和胃底组成 His角(为锐角)而形成的抗反流“阀瓣”。
另外,胃食管低动力状态是GERD的主要动力学特征,也是胃食管反流常见的诱发或加重因素。同样,食管酸清除能力,食管黏膜组织抵抗力和胃排空延迟均是导致GERD的原因。
02 临床表现
GERD临床表现多样,包括食管综合征和食管外综合征,这些表现可单独出现,也可伴随出现。
大部分GERD患者有特征性的临床表现,即烧心、反酸及反食,胸骨后痛,这些都是典型症状。而一部分患者可表现为非典型症状,咽喉部异物感、呼吸道症状、唇舌烧灼感、耳鼻喉相关疾病等等。
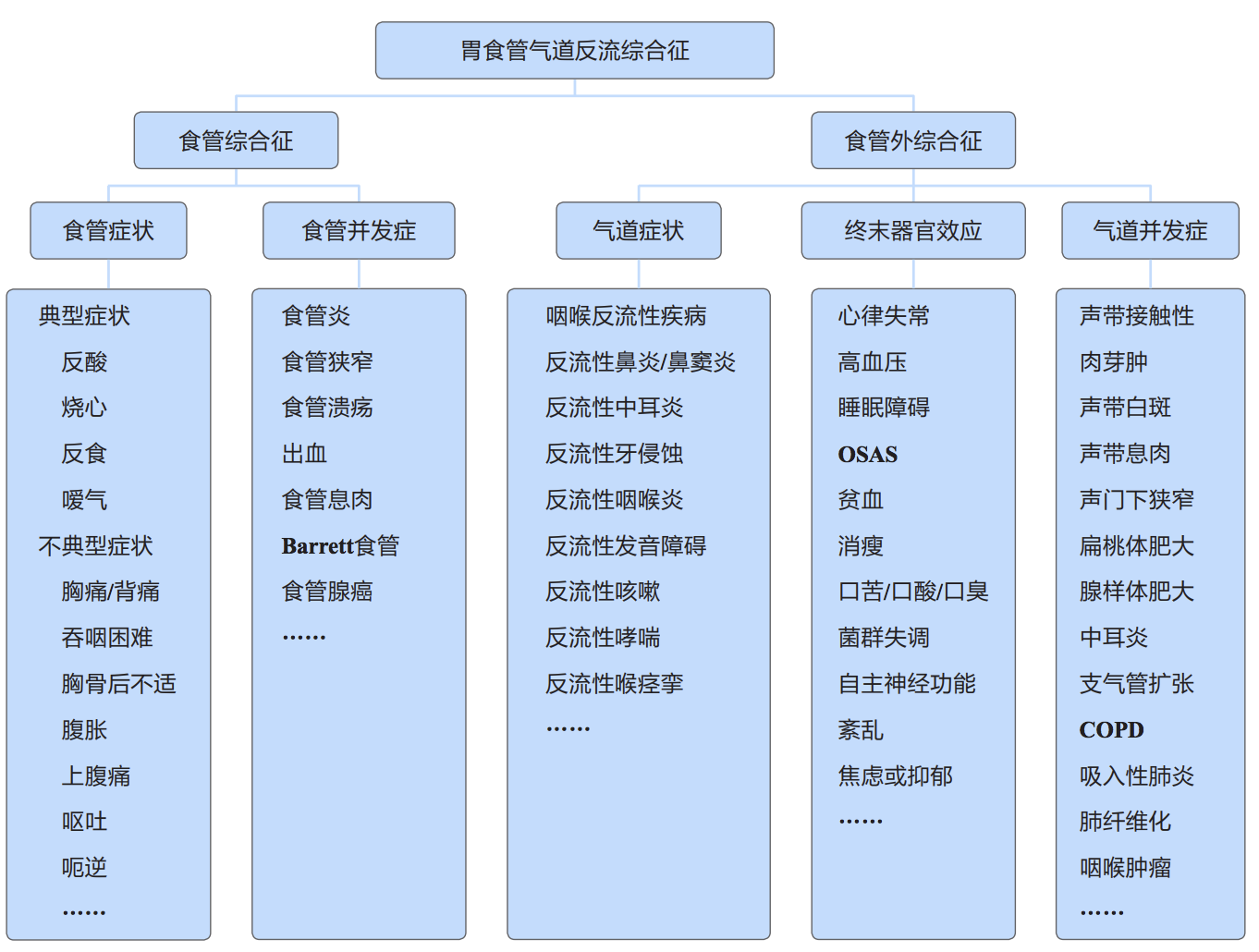
图:胃食管气道反流综合征的临床表现
因此,GERD的临床表现在不同患者间差异较大,是 一种异质性很高的疾病。当患者有“报警”症状时,应积极进行相应检查,排除器质性疾病。
03 治疗
对于GERD的治疗,主要以控制症状、治愈食管炎、减少复发、防止并发症为主。目前,GERD治疗方式包括改善生活方式、药物治疗和手术治疗。
1)改善生活方式
生活调理和疾病的科普教育是GERD治疗和预防的基础,无论采取何种治疗方法,生活调理应贯穿始终。
具体而言,GERD患者餐后容易导致反流,故睡前不宜进食,白天进食后不宜立即卧床,应注意减少一切影响腹压增高的因素,比如肥胖、便秘、咳嗽、呕吐、穿紧身衣等。另外,在饮食中,应降低高脂肪、巧克力、咖啡、浓茶等摄入,需戒烟限酒。
对于老年患者,因LES功能减退容易出现胃食管反流,若同时合并有心血管疾病而服用硝酸甘油制剂或钙离子通道阻滞剂可加重反流症状,应当避免。同时,支气管哮喘患者如合并胃食管反流可加重或诱发哮喘症状,应尽量避免茶碱及肾上腺素受体激动剂。
2)药物治疗
药物治疗是GERD的一线疗法,而在药物应用时,必须注意评价疗效,即食管炎的分级情况、严重程度及发作频率。此外,长期用药的患者需警惕和监视药物不良反应。
目前,GERD治疗的常用药物包括抑酸剂、抗酸剂、 促胃肠动力药、黏膜保护剂、胆汁结合剂、神经调节剂和中药等。PPI是治疗GERD的首选药物,可迅速缓解大部分患者的症状,逆转部分GERD并发症。同时,为了获得最佳疗效,以上药物常联合使用。
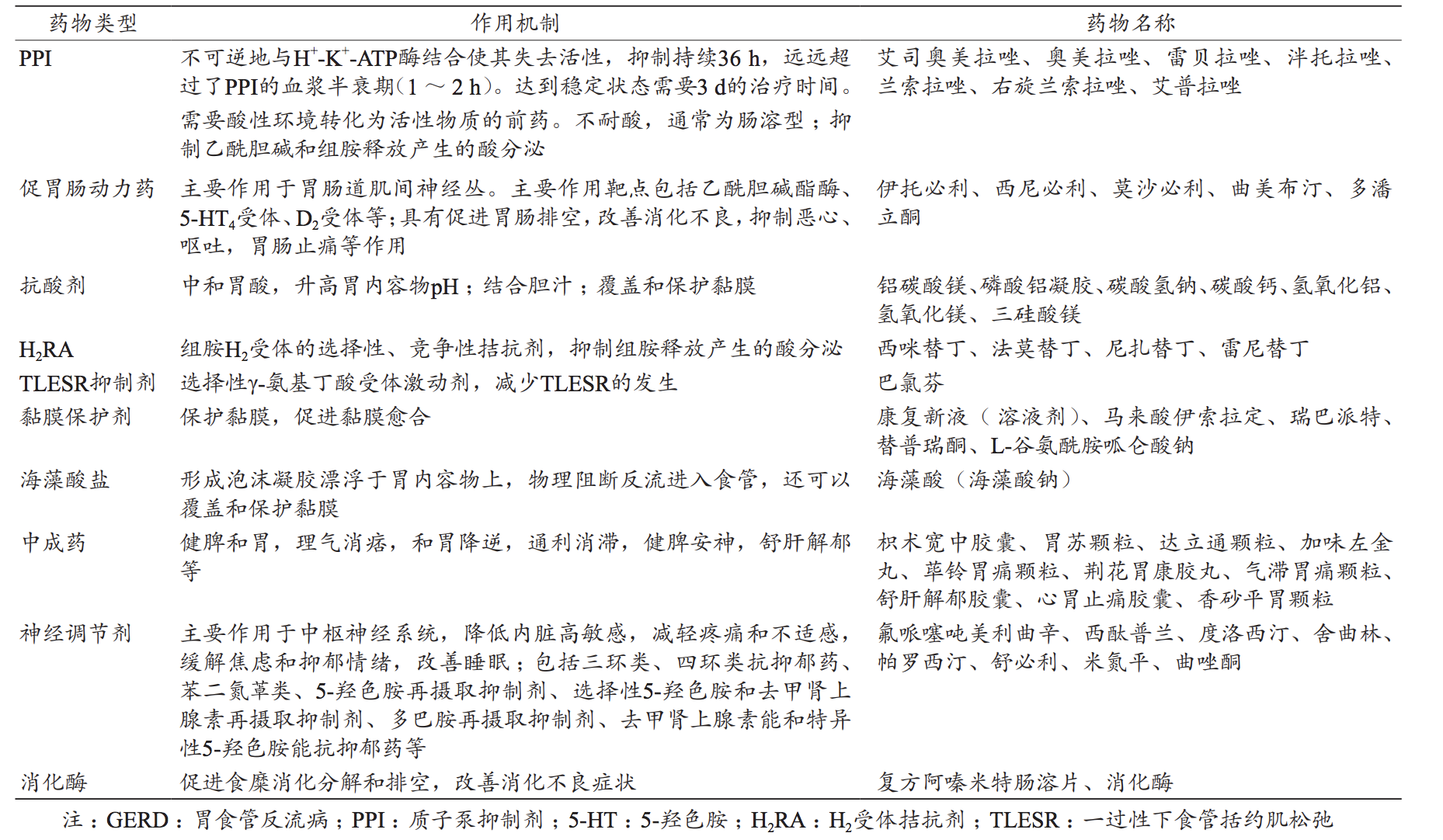
图:GERD的治疗药物及其作用机制
PPI在绝大部分患者中比较安全,不良反应少见,消化不良、恶心、腹泻、呕吐、疼痛、过敏、 粒细胞减少等在用药初期即可发现。然而,合并糜 烂性食管炎、消化性狭窄、Barrett食管、向心性肥胖、HH和部分食管外反流患者需长期服用PPI,应重视长期使用PPI的可能风险。
3)手术治疗
对胃食管反流的手术治疗一般持谨慎态度,需要权衡利弊。以下情况可考虑手术治疗:
1、经过内科治疗症状和食管炎仍然严重的患者;
2、药物治疗有效但需要长期维持治疗,手术治疗主要是避免长期药物负担和潜在风险;
3、经扩张治疗后反复发作的消化性食管狭窄者;
4、合并明显食管裂孔疝者;
5、过去抗反流手术失败者;
目前,抗反流手术的方式主要是不同术式的胃底折叠术。腹腔镜下抗反流手术在我国尚处于推广阶段,医生需要大量的规范化培训,以保证手术成功率、减少术后复发和并发症。
当前,标准的抗反流手术为腹腔镜食管裂孔疝 修补术+胃底折叠术,常用术式包括完全胃底折叠(Nissen,360˚折叠)和部分胃底折叠(Toupet, 270˚折叠和Dor,180˚折叠),完全和部分胃底折叠的疗效相似。据数据显示,GERD典型症状的手术有效率达90% 以上,食管外症状抗反流手术的有效率达 80%以上。
此外,内镜下治疗是介于药物治疗和手术治疗的一 种非常简便、微创的抗反流治疗方式,虽然有效率低于腹腔镜抗反流手术,但有其适用的特定人群, 可替代部分患者的药物治疗或手术治疗。
综上,GERD对于不同个体,有着不同症状的描述,多个症状的严重程度、频率、加重和缓解规律,患者需要个体化管理。近年来,随着人们对GERD认识越来越深刻,多学科联合诊疗模式为其全面的诊治提供了良好的基础,也成为成功诊治GERD的关键。
参考资料
1,吴继敏, 汪忠镐, 胡志伟,等. 中国胃食管反流病多学科诊疗共识[J]. 中华胃食管反流病电子杂志 2020年7卷1期, 1-28页, 2020.
2,于皆平, 沈志祥, 罗和生. 实用消化病学[J]. 世界华人消化杂志, 2007, 8(003):281.
3,中国医师协会消化医师分会胃食管反流病专业委员会,中华医学会消化内镜学分会食管疾病协作组.2020年中国胃食管反流病内镜治疗专家共识[J].中华消化内镜杂志,2021,38(1):1-12.
4,Gyawali C.Prakash,Fass Ronnie.Management of Gastroesophageal Reflux Disease.Gastroenterology 2018,154,302-318.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胃食管#
53
学习了
37
学习了
51
#胃食管反流#
58
#食管#
39
#反流#
41
学习了
42