JAMA Surg:治疗前CEA水平有助于评估结肠癌5年生存率
2015-07-09 沐晴 MedSci原创
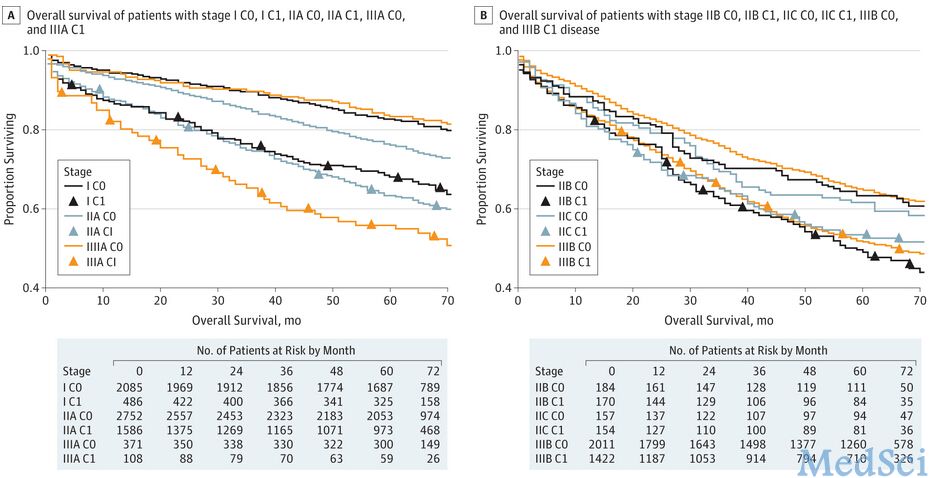
研究意义:美国癌症联合会(AJCC)提议将治疗前血清CEA水平(C 期),列入传统的结肠癌TNM分期系统中。这项提议尚未被广泛采纳,因为目前仍缺乏有关将治疗前CEA水平(C 期)列入AJCC分期系统后,结肠癌长期生存率的研究。 研究目的:为了评估将C期纳入标准的AJCC TNM分期,对长期的总生存率和癌症生存率的影响,进一步探究这项提议对评估生存期的意义。 研究设计:我们从国家癌症协会
研究意义:美国癌症联合会(AJCC)提议将治疗前血清CEA水平(C 期),列入传统的结肠癌TNM分期系统中。这项提议尚未被广泛采纳,因为目前仍缺乏有关将治疗前CEA水平(C 期)列入AJCC分期系统后,结肠癌长期生存率的研究。
研究目的:为了评估将C期纳入标准的AJCC TNM分期,对长期的总生存率和癌症生存率的影响,进一步探究这项提议对评估生存期的意义。
研究设计:我们从国家癌症协会监管所(NCIS)的流行病学调查和最终结果汇总的数据库中,选择自2004年1月至2005年12月31日之间,在病理组织学上确诊为结肠恶性肿瘤的所有患者,进行回顾性研究。我们基于患者治疗前的血清CEA水平,将AJCC分期分为,C0(正常)或者C1(升高)。回访期中位值为71个月。主要评估结果:使用5年总生存率和疾病相关生存率及危险比(HRs)来评估总死亡率和疾病相关死亡率。
1.44-1.59;P < .001)和59%(HR, 1.59; 95% CI, 1.49-1.69;P < . 001) 。对AJCC 的举措——将TNM分期细分的C0 或C1期进行分析,可以看出,与C0期相比,C1期预后更差。这种生存率方面的改变,会诱发一波对其他AJCC肿瘤C0或C1生存率的评估。对处于I,II,III阶段的癌症患者进行分析,结果显示淋巴结阴性的C1期疾病与淋巴结阳性的C0期预后相似或更差。
结论和相关性:把C期列入AJCC TNM 结肠癌分期,显示根据五年生存率来评估C期的话,C0和C1期存在很大差异。将C期进行细分,可以引起疾病生存率评估的实质性变化。C1期预示着与AJCC TNM更高层分期相似或更糟糕的预后。我们推荐进一步开展前瞻性的随机临床试验,将治疗前的CEA检测水平作为结肠癌治疗的标准,同时使用将C期进行分期,开展多种模式的治疗计划和风险分层。
原始出处:
Pretreatment Serum Carcinoembryonic Antigen Levels Into AJCC Staging for Colon
Cancer on 5-Year Survival. JAMA Surg.2015 Jun 17. doi:
10.1001/jamasurg.2015.0871.[PDF free]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












可以为结肠癌分期提供参考
102
将已有的资源运用到极致!
118
很有用
108
看看
121
#生存率#
29
#CEA#
34
看看
91