CHEST:OSA的严重程度是房颤发生的独立预测因子
2015-11-02 崔倩 译 MedSci原创
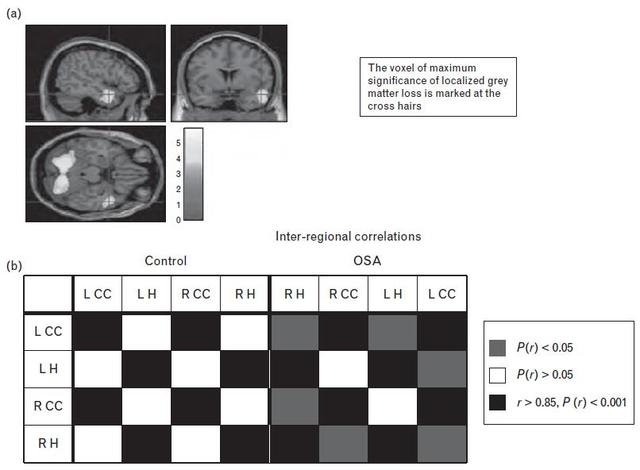
OSA已经是和房颤(AF)相关的常见现象,但来自大型纵向队列数据建立OSA是否是AF独立于肥胖和其他已经建立风险的风险因素的数据还很少。研究人员在1989年和2001年间招募了患者参与睡眠门诊简称为实验室多导睡眠图监测可能的OSA。1970年至2009年之间西澳大利亚全部的人群住院数据被链接到睡眠研究病例中,以确定住院治疗至2009年AF事件。Cox回归分析被用来评估OSA与事件AF的独立相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Chest#
35
#EST#
33
#预测因子#
32
#OSA#
43