CHEST:中重度OSA与冠状动脉粥样斑块体积相关
2014-02-17 sd3212 dxy
虚拟组织学血管内超声(VH-IVUS)是一种血管内成像技术,可评估冠状动脉内粥样硬化斑块的特征。为了了解冠状动脉疾病患者中,阻塞性睡眠呼吸暂停(OSA)与其冠状动脉内粥样硬化斑块特征之间的联系,来自新加坡国立大学心脏中心心脏科的Lee博士等进行了一项研究,研究结果在线发表于2013年10月31日的CHEST杂志上。结果显示在患有冠状动脉疾病的患者中,中度至重度OSA是目标冠
虚拟组织学血管内超声(VH-IVUS)是一种血管内成像技术,可评估冠状动脉内粥样硬化斑块的特征。为了了解冠状动脉疾病患者中,阻塞性睡眠呼吸暂停(OSA)与其冠状动脉内粥样硬化斑块特征之间的联系,来自新加坡国立大学心脏中心心脏科的Lee博士等进行了一项研究,研究结果在线发表于2013年10月31日的CHEST杂志上。结果显示在患有冠状动脉疾病的患者中,中度至重度OSA是目标冠状动脉粥样斑块总体体积较大的独立相关因素。【原文下载】
该研究是一项前瞻性临床研究,其研究对象主要是经血管造影证实为患有冠状动脉疾病的患者,进行VH-IVUS检查、和以家中睡眠为主的睡眠研究,并测量整个目标冠状动脉内动脉粥样斑块的总体积,及其薄纤维帽粥样硬化斑块的发生率;此外,对无OSA、及合并轻度OSA患者,与合并中度~重度OSA患者之间指标的差异进行比较。
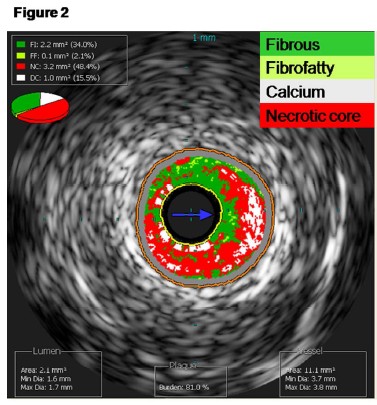
研究共招募了118例受试者,其中93例完成了研究,共有32 例(34.4%)被新诊断为轻度~重度OSA,其呼吸暂停低通气指数(AHI)均>15.与无OSA、及合并轻度OSA组患者相比,合并中度~重度OSA患者动脉粥样硬化斑块的总体积明显更大,并具有统计学意义上的显著性差异。
而且这种差异在对受试者年龄、体重指数、高血压、糖尿病、吸烟、以及高脂血症等因素进行了统计学校正后依然存在。相反,两组受试者薄纤维帽粥样硬化斑块的发生率则分别为53.1%与54.2%,不具有显著性差异。
该研究结果显示,在患有冠状动脉疾病的患者中,中度至重度OSA是目标冠状动脉粥样斑块总体体积较大的独立相关因素。研究者认为,有必要在未来的研究中,进一步评估连续气道正压通气治疗对于此类患者动脉粥样斑块总体体积的影响。
原始出处:
Tan A, Hau W, Ho HH, Ghaem Maralani H, Loo G, Khoo SM, Tai BC, Richards AM, Ong P, Lee CH.OSA and Coronary Plaque Characteristics.Chest. 2014 Feb 1;145(2):322-30. doi: 10.1378/chest.13-1163.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Chest#
42
#动脉粥样斑块#
32
#粥样斑块#
44
#EST#
34
#斑块#
29
#OSA#
36